The medial side of the upper arm is supplied by perforator arteries arising from the brachial artery, the superior ulnar collateral artery and the artery to the biceps muscle. Fasciocutaneous flaps from the medial arm region could be designed based on these perforating arteries, but the anatomical variability of this region has led to a loss of interest in it as a donor area for fasciocutaneous flaps.
The aim of this study is to identify, through cadaveric dissection, whether there are constant perforator arteries from the brachial artery that could be used to raise fasciocutaneous flaps from the inner side of the arm.
For this purpose, 15 upper extremities belonging to body-donors have been dissected. Six extremities were right-side arms and six belonged to female donors. 7 parameters and the differences between gender and side of the upper extremity were studied (distances from the acromion and the coracoid to the beginning and to the end of each perforating artery, distance from the insertion of the distal tendon of the biceps muscle to the origin of each perforator artery, length and diameter of the perforators arteries).
Perforator arteries arising from the brachial artery to the inner face of the arm were found in all the upper limbs dissected. The median number of these perforator arteries found by the upper limb was 5±1.9 (range 3-9). Anatomical variations consisted of the number of perforator arteries that were found in each limb. Only in 2 arms (13.3%), the perforator arteries arose from a superficial brachial artery or from the distal part of the brachial artery. The mean diameter of the perforating artery was 1.80±0.58 mm, and the mean length resulted in 4.67±2.07 cm.
The consistent vascular anatomy found for these perforator arteries, arising from the brachial artery, and the easy landmarks described justify the use of fasciocutaneous flaps of the medial side of the arm for reconstructive surgery.
The medial arm fasciocutaneous flap: a wasted alternative?
A.M. Vidal1, José R. Sañudo2, S. Quinones2, Marko Konschake3, R. García-Pumarino1, Paloma Aragonés2,4
1 Department of Obstetrics and Ginecology, Cantonal Hospital Lucerne, Switzerland
2 Department of Human Anatomy and Embryology, Universidad Complutense, Madrid, Spain
3 Department of Anatomy, Histology and Embriology, Medical University of Innsbruck, Innsbruck, Austria
4 Orthopedics Department, Hospital Universitario Santa Cristina, Madrid, Spain
SUMMARY
Sign up or Login
INTRODUCTION
The brachial artery (BA) is the continuation of the axillar artery, and begins at the level of the lower border of the teres major muscle. This vessel runs along the medial aspect of the arm, crosses the long and medial heads of the triceps muscle, the coracobrachialis muscle, passes on to the brachial muscle and reaches the deep face of the bicipital aponeurosis in the elbow (Cormack and Lamberty, 1994).
Cormack and Lamberty (1994) described the vascularization pattern of the medial side of the upper arm. According to these authors, this region is supplied by a row of 5 or 6 perforators arising from three sources: the BA, the superior ulnar collateral artery (SUCA) and the artery to the biceps.
The concept that the cutaneous vessels consistently perfuse their own specific areas of the skin was firstly proposed by Manchot: he attributed the vascularization of the medial aspect of the arm to the SUCA and its cutaneous branches (Manchot, 1889). Afterwards, Michel Salmon reviewed Manchot’s works with the aid of X-ray (Salmon, 1930).
Later, the cutaneous vascular supply of the inner arm was studied, and it was seen that it derived from branches of the brachial artery (BA). These can either branch off the BA directly or indirectly via branches of the SUCA, inferior ulnar collateral artery (IUCA) or superficial brachial artery (SBA) (Lippert and Pabst, 1985; Taylor and Palmer, 1987).
On the medial side of the upper arm, fasciocutaneous flaps and neurovascular free flaps may be based on a single large fasciocutaneous perforator (Cormack and Lamberty, 1994). In recent years, there has been a need to increase the research in the vascular anatomy of the arm skin and the possibility of employing flaps of perforating arteries in reconstructive surgery.
With increasing clinical utilization of cutaneous flaps, there has been new anatomic knowledge of the flaps, blood supplies, and designs (Le Huec et al., 1995; Cormack and Lamberty, 1994; Hwang et al., 2005), but the data on the fasciocutaneous vascularisation of the medial aspect of the arm are incomplete in the literature. The number, situation and variable caliber of the musculocutaneous perforators do not allow for any classification (Le Huec et al., 1995).
Discrepancies between reports on vascular anatomy and a variability of terminology have also made the medial upper arm blood supply unclear (Matloub et al., 1992; Hwang et al., 2005; Karamürsel et al., 2005). Subsequently, the use of fasciocutaneous flaps from the inner face of the arm has lost interest.
Thus, the purpose of this descriptive anatomical study was to report the anatomy of the perforating arteries (PA), originating from the BA as a possible option for axillary reconstruction, and to propose the possible surgical approach based on the fasciocutaneous flap of the inner side of the arm.
MATERIAL AND METHODS
To conduct this descriptive study, the authors employed 15 upper extremities belonging to body-donors from the Department of Human Anatomy and Embryology of the Medical Faculty, Universidad Complutense of Madrid (Spain).
Of the 15 extremities, six belonged to three previously fixed cadavers preserved with 10% formaldehyde. The nine remaining extremities belonged to various unfixed fresh cadavers. Six extremities were right-side arms, and nine were left arms. Six belonged to female donors, and nine to male donors.
Anatomical dissection was performed as follows: firstly, the authors delimited the skin area of interest, continued with the dissection and traction of the skin and subcutaneous cell tissue, until the biceps brachii muscle was reached. The terminal branches of the brachial plexus—the medial antebrachial cutaneous nerve, the median nerve and ulnar nerve—and the vascular elements—the brachial veins and the brachial arteries—were identified.
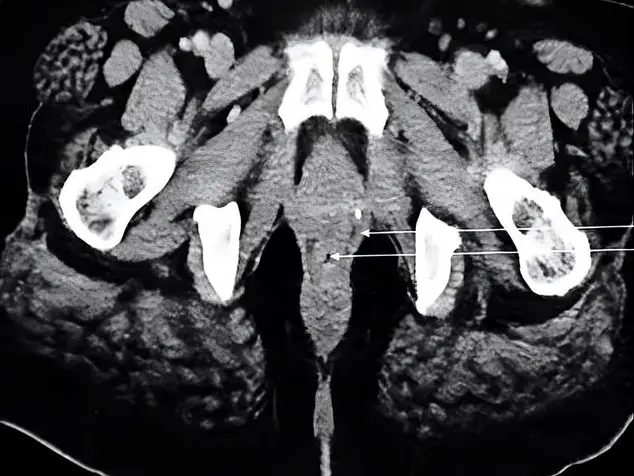
The proximal part of the brachial artery was located and a thorough dissection of it was started to reach the perforating arteries, and continued until its multiple branches reached the subcutaneous cellular tissue of the inner face of the arm (Figs. 1, 2 and 3).
Seven parameters and the differences between gender and side of the upper extremity were studied (Fig. 4):
Distance from the coracoid process to the origin of the perforating artery from the brachial artery (A).
Distance from the acromion to the origin of the perforating artery from the brachial artery (B).
Distance from the coracoid process to the end perforating artery (C).
Distance from the acromion to the end perforating artery (D)
Distance from the insertion of the distal tendon of the biceps muscle to the origin of the perforating artery (E).
Diameter of the perforating artery at the origin from the BA (F).
Length of the perforating artery (G).
The results were treated statistically with IBM SPSS Statistics.
RESULTS
Of the 15 upper extremities, 40% belonged to female body-donors and in 40% of the cases the side was right.
Septocutaneous PA arising from the BA to the inner face of the arm were found in all the upper limbs dissected. The median number of PA arising from the BA found by upper limb was 5±1.9 (range 3-9). Anatomical variations consisted of the number of PA that were found in each limb. Only in 2 arms (13.3%), the PA arosed from a superficial brachial artery or from the distal half of the BA.
For each of the parameters A, B, C, D and E, the mean distance (MD) and the standard deviation (SD) in cm were calculated. The results have been represented in Table 1.
Table 1. Mean distance and standard deviation calculated for parameters A, B, C, D and E.
|
Parameter measured |
|||||
|
A |
B |
C |
D |
E |
|
|
Mean distance (cm) |
15.2 |
13.38 |
16.37 |
18.44 |
10.01 |
|
Standard deviation (cm) |
3.07 |
3.39 |
2.77 |
2.77 |
2.73 |
The mean diameter and SD of the perforating artery (parameter F) was 1.80±0.58 mm, and the mean length and SD resulted in 4.67±2.07 cm (parameter G).
The ranges of the measures obtained for parameters A, B, C and D were classified by gender and represented in Table 2.
Table 2. Ranges measured for parameters A, B, C and D for males and females.
|
Parameter measured |
||||||||
|
Males |
Females |
|||||||
|
A |
B |
C |
D |
A |
B |
C |
D |
|
|
Range (cm) |
7.5-22.50 |
11-24.5 |
13-20.5 |
15.5-26 |
7.5-18 |
8- 19.50 |
10-20 |
12.5- 21 |
The minor and major diameters of the perforating artery (parameter F), as well as the maximum and minimum values of its length (parameter G) were also collected and classified by gender (Table 3).
Table 3. Ranges measured for parameters F and G for males and females.
|
Parameters measured |
||||
|
Male |
Female |
|||
|
F |
G |
F |
G |
|
|
Range (mm) |
1-3 |
20-65 |
1-3 |
25-100 |
Among the sample, 3 different patterns of origin of the PA were found:
Pattern A. The PA branches off from the upper part of the brachial artery. This was found in 12 upper extremities (80%).
Pattern B. The PA branches off from the inferior part of the brachial artery. 2 upper extremities presented this pattern (13.3%).
Pattern C. 1 upper extremity of the sample presented 2 brachial arteries, a superficial and a deep one. The PA arose from the superficial brachial artery (6.7%).
DISCUSSION
According with the findings of Cormack and Lamberty (1994), the skin in the medial region of the arm is supplied by 5 or 6 perforating arteries that cross the deep fascia of the arm. These fasciocutaneous perforating arteries range from the brachial artery, the superior ulnar collateral artery and the artery to the biceps.
Origin and distribution of the perforator arteries of the medial arm have been investigated in several reports. Some authors (Dolmans et al., 1979; Kaplan and Pearl, 1980; Gao et al., 1985; Breidenbach et al., 1987; Bhattacharya et al., 1991; Matloub et al., 1992; Le Huec et al., 1995; Mathes and Nahai, 1996) have suggested a predominant role of the superior ulnar collateral artery (SUCA) and its branches for the blood supply of the medial aspect of the arm, while others have defended the role of the brachial artery (Manchot, 1983; Zbrodowsky et al., 1987; Carriquiry, 1990; Karamürsel et al., 2005; Yakup et al., 2010).
Manchot (1983) described several branches arising from the BA that irrigate the anteromedial skin of the arm, and also in 1987 direct cutaneous arterial branches from the BA were reported (Zbrodowsky et al., 1987). Yakup et al. (2010), after a study of 14 body donors’ upper limbs, described a constant perforator branch from the BA that supplied the distal medial skin of the arm. Carriquiry (1990) confirmed, in 14 dissected upper limbs, that direct septocutaneous branches from the BA were the main source of irrigation of the skin of the medial arm, while the branches arising from the SUCA tend to distribute in the skin more posteriorly than the BA branches do.
In a recent publication with a sample of 20 body donors’ upper limbs, the authors found that the skin of the distal third and the proximal third of the medial arm was mostly supplied by perforator branches of the BA and the intermediate third by perforators of the SUCA and the BA anteriorly and by the SUCA posteriorly (Perignon et al., 2013).
Our anatomical study focused on the perforating arteries of the medial upper arm that arose from the brachial artery. The finding of a PA from the BA was constant in our entire sample, which ensures an easy and predictable dissection. The median number of PA from the BA found in each upper limb was 5±1.9 (range from 3-9). These findings coincide with those of Cormack and Carriquiry, who found several septocutaneous branches from the BA along the medial septum at different levels (Cormack and Lamberty, 1994; Carriquiry, 1990). Moreover, Tinhofer found in 20 upper limps from fresh cadavers, an average of 4.556±1.47 PA arose from the BA (Tinhofer et al., 2017).
The mean diameter of the PA from the BA in our sample was 1.80±0.58 mm (1-3 mm), while the mean length resulted in 4.67±2.07 cm (2-10 cm) (Table 3). Other authors have measured these parameters of the PA arising from the BA; the internal diameters of these PA described by Cormack and Lamberty (1994) range from 0.2 mm to 1.2 mm. Tinhofer et al. (2017) defined a mean diameter of 0.68±0.27 mm and their pedicles had an average length of 3.62±1.61 cm.
Perignon et al. (2013) reviewed the first PA of the BA and found a mean diameter of 1 ± 0.44 mm (0.5-1.8 mm), and a mean length of 3.5 ± 1.06 cm (2-6 cm). Yakup et al. (2010) and Hwang et al. (2005) described the distal brachial artery’s main perforator as a constant PA of the BA with a mean diameter of 0.95 mm and 0.94 mm, and a mean length of 3.3 cm and 2.78 cm, respectively.
We measured in our cadaveric sample the distance from the coracoid to the origin of the PA from the BA (parameter A), and the values found were 15.2±3.07 cm, with a range of 7.5-22.5 cm. The distance from the acromion to the origin of the Pa from the BA (parameter B) was also measured and the values were 13.38±3.09 cm, with a range of 8-24.5 cm (Tables 1 and 2). Other authors measured, in body donors’ upper limbs, the distance from the medial epicondyle to the first PA of the BA and found a distance of 19±2.69 cm (11.5-23 cm) (Perignon et al., 2013). Carriquiry (1990) described 3 to 4 septocutaneous branches arising from the BA along the medial septum, the uppermost one was close to the lower border of the pectoralis major tendon and the lowermost branch was located 2 to 4 cm above the medial epicondyle.
The medial upper arm flap was first described by Daniel et al. in 1975 for hand reconstruction in a 25-year-old man, but it was not finally attempted. This neurovascular island flap was designed based on the medial brachial cutaneous nerve and superficial branch of the SUCA, with its venae comitantes. This superficial artery is a constant artery and its diameter ranges from 0.5 to 1.4 mm. Dolmans et al. (1978) conducted a clinical trial with a neurocutaneous island flap from the medial arm on a patient, but the flap developed venous and arterial thrombosis and failed. It was not until 1979 before the first successful free transfer of the medial arm flap was carried up by Newsom (1979). This author performed a flap from medial arm skin, elevated on the superficial branch of the SUCA, to close a large oronasoantral fistula. The external diameter of the flap artery was 0.8 mm.
Yakup et al. (2010), after a study of 14 body donors’ upper limbs, also advocated the use of a rotating fasciocutaneous flap in the lower part and medial region of the arm, based on a perforating artery arisen from the BA. At least one main PA and one accessory PA from the BA were found in all the extremities.
The medial arm fasciocutaneous flap has been raised in reconstructive surgery as local flap to cover elbow and axillary defects and contractures (Kaplan and Pearl, 1980; Maruyama et al., 1985; Yakup et al., 2010). Also, it has been used as fasciocutaneous free flap for reconstructions of the maxillofacial region, neck and the hand (Newsom, 1981; Song et al., 1981; Le Huec et al., 1995).
Carriquiry (1990) described axillary and elbow crease contractures released with medial arm island flaps, and thumb and hand defects covered in a cross-arm fashion.
The use of this fasciocutaneous flap of the medial arm offers many advantages: the surgical technique is simple and reproducible, the donor area is well-hidden, it can be easy closed in a linear way and it does not cause functional problems (Carriquiry, 1990).
Furthermore, the flap has thin, elastic and hairless skin, making it excellent for face, neck and hand reconstructions (Kaplan and Pearl, 1980). It also has better color match for head and neck reconstructions (Carriquiry, 1990).
As other authors have already described (Carriquiry, 1990), we propose the use of this fasciocutaneous flap based on PA from the BA as free flap to cover axillary defects. Specifically, we think that it could be a good surgical solution for the definitive treatment of hidradenitis suppurativa and for contractures after large deep burns.
Unfortunately, despite the great advantages described, the inner side of the arm appears to be frequently ignored in the choice of a potential flap due to the wider distribution of the PA from the medial intermuscular septum than the ones from the lateral intermuscular septum (Hwang et al., 2005).
We describe in our sample the PA arising from the BA, and we found them in a number of 3 to 9. The consistent vascular anatomy found for these PA and the easy landmarks described justify the use of fasciocutaneous flaps of the medial side of the arm for reconstructive surgery.
The only cases of anatomical variations in our study are due to an increase in the number of perforating arteries, and only in 2 (13.3%) of the cadavers the PA arose from the distal region of the brachial artery or from a superficial brachial artery. Instead of our findings, Yakup et al. (2010) described a distal brachial artery main perforator vessel in a sample of 14 upper limbs, and this vessel was seen in all dissected cadavers, and other authors found only one constant medial PA from the BA in the arm, located 8.9cm proximal to the medial epicondyle (Hwang et al., 2005).
Although in our study we can prove the presence of PA from the BA in a number from 3 to 9 in each limb, due to the variability described in the literature reviewed we recommend the use of a preoperative CT-angiography or Doppler ultrasound for surgical safety.
Conclusions
The fasciocutaneous flap of the medial based on PA from the BA can be raised safely and easily. Our study find that these PA appear constantly and provides anatomical references to locate these vessels in order to be applied clinically.
This flap provides advantages such as thin, elastic and hairless skin, in addition to being a well-hidden donor area without functional alterations.
ACKNOWLEDGEMENTS
To Dr. T. Vázquez (Director) and to the Technical Staff of the Center of Donors of Cadavers and dissecting Rooms of the Universidad Complutense of Madrid, Spain.
DECLARATIONS
Funding
The authors have no financial or personal relationship with any third party whose interests could be positively or negatively influenced by the article’s content. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
The cadavers belonged to the Donors and Dissecting Rooms Center, Universidad Complutense de Madrid, Spain. The bodies were under a strict control by the ethical committee in accordance to the ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all the participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figures 1, 2, 3 and 4.
Related articles
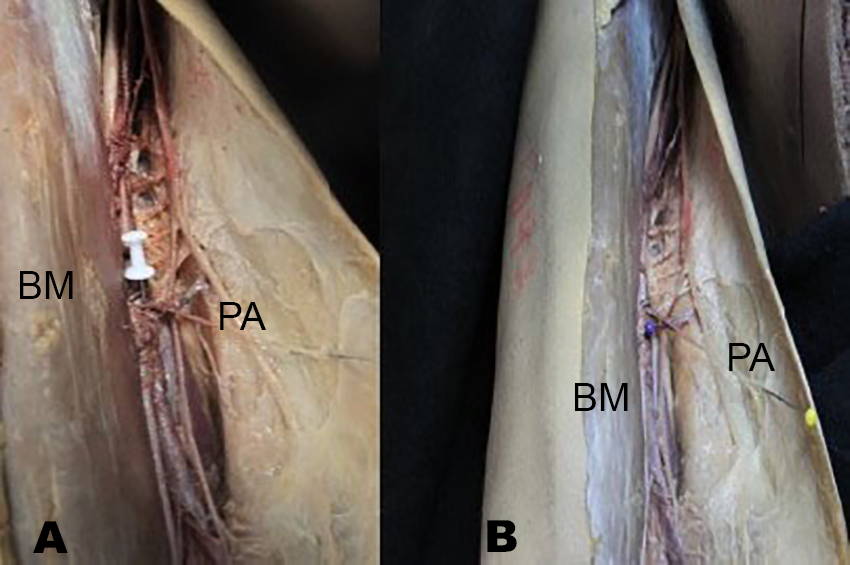 Fig. 1.- A: Right upper limb of a formolated body donor. The white pushpin points out the origin of the perforator artery (PA) from the brachial artery. B: Right upper limb of a formolated body donor. The blue pushpin points out the brachial artery and the origin of a PA. The yellow pushpin shows the PA. BM: biceps muscle.
Fig. 1.- A: Right upper limb of a formolated body donor. The white pushpin points out the origin of the perforator artery (PA) from the brachial artery. B: Right upper limb of a formolated body donor. The blue pushpin points out the brachial artery and the origin of a PA. The yellow pushpin shows the PA. BM: biceps muscle. 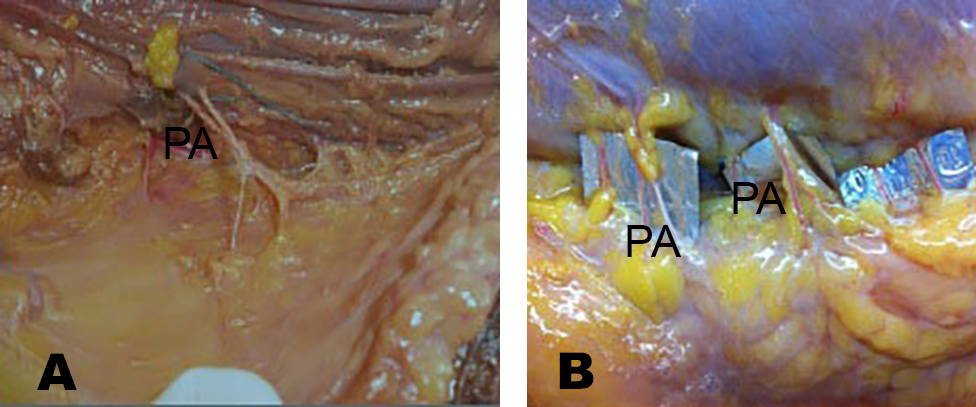 Fig. 2.- A, B: Left upper limb of a fresh cadaver. Various perforator arteries (PA) can be observed arising from the brachial artery and reaching the deep fascia.
Fig. 2.- A, B: Left upper limb of a fresh cadaver. Various perforator arteries (PA) can be observed arising from the brachial artery and reaching the deep fascia.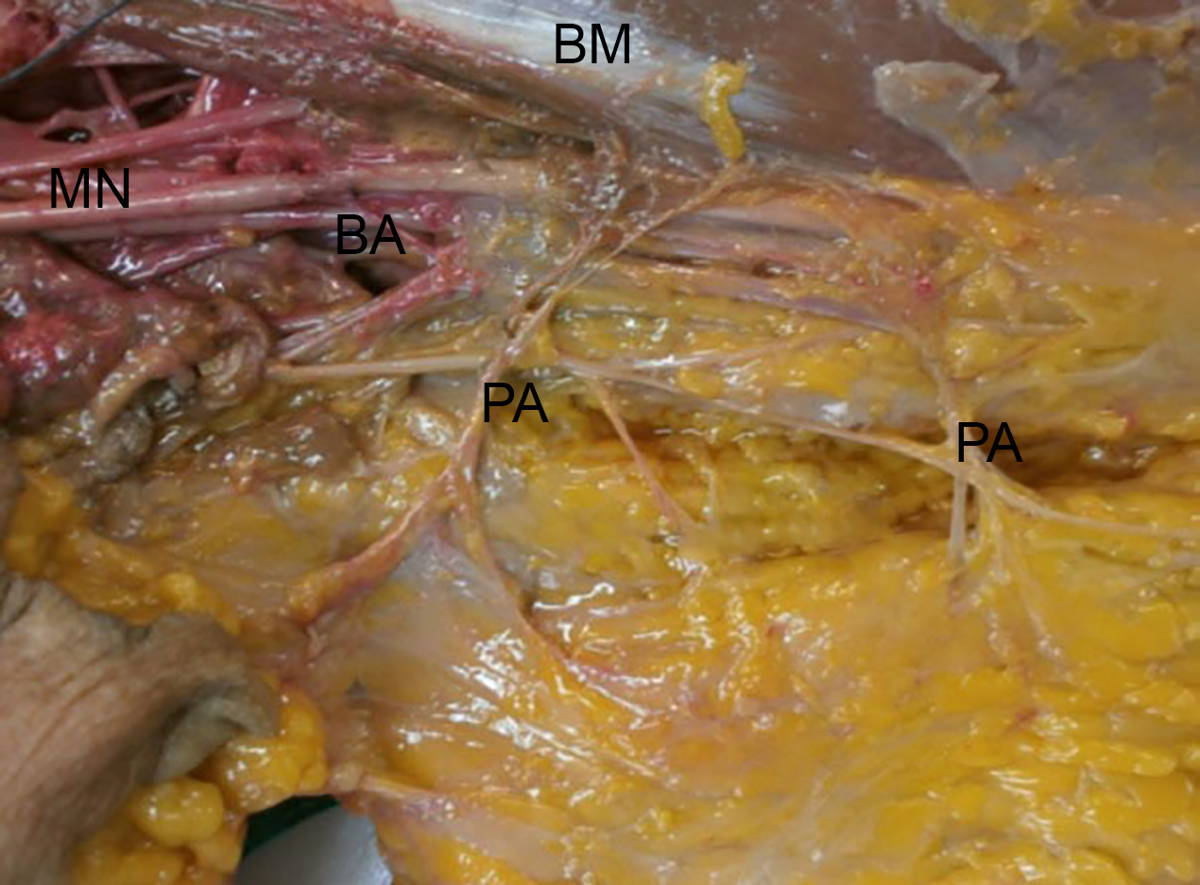 Fig. 3.- Left upper limb of a fresh cadaver. Perforator arteries (PA) arise from the brachial artery (BA) and reach the deep fascia of the inner side of the arm. BM: biceps muscle, MN: median nerve.
Fig. 3.- Left upper limb of a fresh cadaver. Perforator arteries (PA) arise from the brachial artery (BA) and reach the deep fascia of the inner side of the arm. BM: biceps muscle, MN: median nerve.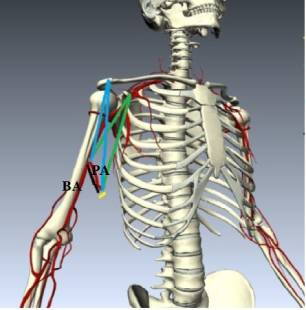 Fig. 4.- Diagram of a perforator artery arising from the brachial artery of a right upper limb. The brachial artery (BA) is shown with its perforating artery (PA) towards the inner side of the arm. Blue lines: distance from the acromion to the origin of the perforating artery from the brachial artery (parameter B) and distance from the acromion to the end of the PA (parameter D). Green lines: Distance from the acromion to the origin of the PA from the BA (parameter A) and distance from the acromion to the end of the PA (parameter C). Yellow line: Diameter of the PA (parameter F). Black line: Length of the PA (parameter G).
Fig. 4.- Diagram of a perforator artery arising from the brachial artery of a right upper limb. The brachial artery (BA) is shown with its perforating artery (PA) towards the inner side of the arm. Blue lines: distance from the acromion to the origin of the perforating artery from the brachial artery (parameter B) and distance from the acromion to the end of the PA (parameter D). Green lines: Distance from the acromion to the origin of the PA from the BA (parameter A) and distance from the acromion to the end of the PA (parameter C). Yellow line: Diameter of the PA (parameter F). Black line: Length of the PA (parameter G).BHATTACHARYA S, BHAGIA SP, BHATNAGAR SK, PANDEY SD, CHANDRA R (1991) The medial upper arm fasciocutaneous flap. An alternative flap to cover palmar defects of hand and distal forearm. J Hand Surg Br, 16: 342-345.
BREIDENBACH WC, ADAMSON W, TERZIS JK (1987) Medial arm flap revisited. Ann Plast Surg, 18: 156-163.
CARRIQUIRY CE (1990) Versatile fasciocutaneous flaps based on the medial septocutaneous vessels of the arm. Plast Reconstr Surg, 86: 103-109.
CORMACK GC, LAMBERTY BGH (1994) The arterial anatomy of skin flaps. Ed. Churchill Livingstone, London, England, pp 80, 181-189.
DANIEL RK, TERZIS J, SCHWARZ G (1975) Neurovascular free flaps. Plast Reconstr Surg, 56: 13.
DOLMANS S, GUIMBERTEAU JC, BAUDET J (1979) The upper arm flap. J Microsurg, 1: 162.
GAO X, MAO Z, YANG Z, WANG B (1985) Medial upper arm skin flap: vascular anatomy and clinical applications. Ann Plast Surg, 15: 348-351.
HWANG K, LEE WJ, JUNG CY, CHUNG IH (2005) Cutaneous perforators of the upper arm and clinical applications. J Reconstr Microsurg, 21(7): 463-469.
KAPLAN FN, PEARL RM (1980) An arterial medial arm flap, vascular anatomy and clinical applications. Ann Plast Surg, 4: 205.
KARAMÜRSEL S, BAGDATH D, DEMIR Z, TÜCCAR E, CELEBIOGLU S (2005) Use of medial arm skin as a free flap. Plast Reconstr Surg, 115: 2025-2031.
LE HUEC JC, LIQUOIS F, LEGER O, CHAUVEAUX D, MIDY D, LE REBELLER A (1995) A study of the fasciocutaneous vascularisation of the arm: surgical applications. Surg Radiol Anat, 17(2): 121-128.
LIPPERT H, PABST R (1985) Arterial variations in man: classification and frequency. Bergmann Verlag GmbH, KG; Munich, Germany.
MANCHOT C (1883) The cutaneous arteries of the human body. Springer-Verlag, New York.
MARUYAMA Y, ONISHI K, YOSKIKO Y (1987) The ulnar recurrent fasciocutaneous island flap. Plast Reconstr Surg, 79: 381-387.
MATHES SJ, NAHAI F (1996) Reconstructive surgery. Principles, anatomy and technique. Elsevier, Oxford, pp 747-748.
MATLOUB HS, YE Z, YOUSIF NJ, SANGER JR (1992) The medial arm flap. Ann Plast Surg, 29: 517-522.
NEWSOM HT (1981) Medial arm free flap (Case report). Plast Reconstr Surg, 67: 63.
PERIGNON D, HAVET E, SINNA R (2013) Perforator arteries of the medial upper arm: anatomical basis of a new flap donor site. Surg Radiol Anat, 35: 39-48.
SALMON M (1936) Les arte`res de la peau. Masson, Paris, pp 126-128.
SONG R, SONG Y, YU Y, SONG Y (1982) The upper arm free flap. Clinics Plastic Surg, 9(1): 27-35.
TAYLOR GI, PALMER JH (1987) The vascular territories (angiosomes) of the body: experimental study and clinical applications. Brit J Plastic Surg, 40: 113-141.
TINHOFER IE, TZOU CH, DUSCHER D, POLLHAMMER MS, WENINGER WJ, HUEMER GM, SCHMIDT M (2017) Vascular territories of the medial upper arm-an anatomic study of the vascular basis for individualized flap design. Microsurgery, 37: 618-623.
YAKUP C, KOCABIYIK N, OZTURK S, ISIK S, OZAN H (2010) A new perforator flap from distal medial arm: a cadaveric study. Eplasty, 10: 541-548.
ZBRODOWSI A, MARTI FM, GÜMEWER R, MONTANDON D (1987) Blood supply of the subcutaneous tissue of the upper limb and its importance in the subcutaneous flap. J Hand Surg, 12B: 189.