The most common pattern of hepatic arterial anatomy includes the left and right hepatic artery, both branching from the proper hepatic artery. We present a case where an additional, accessory hepatic artery, originating from the gastroduodenal artery, was found during anatomical dissection. The described artery enters porta hepatis separately, not following the left or right hepatic artery, which may implicate that the accessory artery provides arterial supply for the region defined as segments IVa and IVb (according to Couinaud’s liver segment classification). Such an extremely rare variation of liver vascularization is poorly described in the literature, and it is not included in any of the currently valid classifications. The accessory artery presented in our case could be significant in clinical settings due to its impact on the outcome of surgical procedures.
Rare variant of hepatic arterial supply: a cadaveric case report with a literature review
Domagoj Ivanković 1*, Andrea Blažević 2*, Dominik Vicković 1, Danko Mikulić 3
1 School of Medicine, University of Zagreb
2 Department of Anatomy and Clinical Anatomy, School of Medicine, University of Zagreb
3 Division of Abdominal Surgery and Organ Transplantation, Department of Surgery, University Hospital Merkur, Zagreb
SUMMARY
Sign up or Login
INTRODUCTION
Hepatic arterial anatomy has been the subject of many studies in recent literature. According to the literature, the incidence of hepatic artery anatomical variations ranges from 20 to 50% (Fonseca-Neto et al., 2017). Most typically, the common hepatic artery is a branch of the celiac trunk. After branching of the gastroduodenal artery, the common hepatic artery continues its course as the proper hepatic artery. Then it bifurcates into the left and right hepatic artery, which then enter the liver through the porta hepatis. Multiple possible variants were classified in 1966 by Michels. Michels and colleagues performed a study on 200 dissections and classified variants into ten categories (Michels, 1966). Later, Michels’ classification was modified by Hiatt’s classification, in which six categories were defined (Noussios et al., 2017). However, according to the available literature and in addition to our finding, there are some variations of hepatic arterial vascularization that still cannot be entirely classified. Being familiar with these is crucial in surgical procedures relating to hepatobiliary and pancreatic surgery. We report a variant that is not described by either Michels’ or Hiatt’s classification.
CASE REPORT
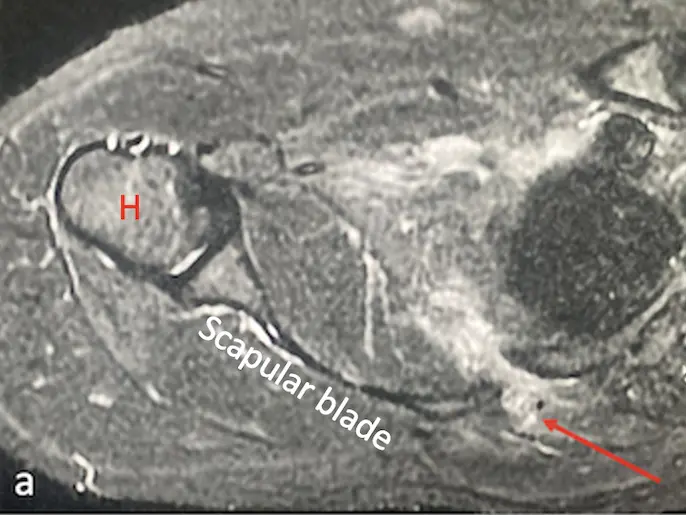
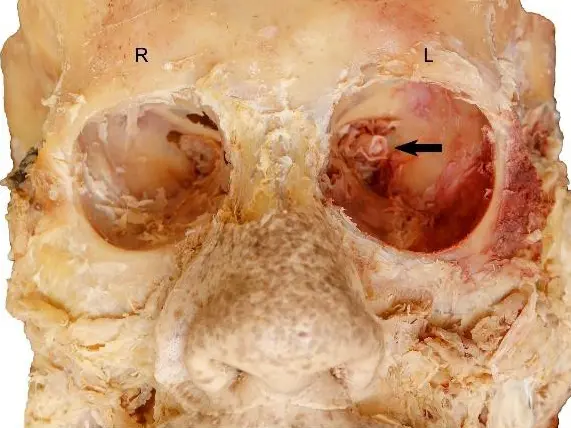
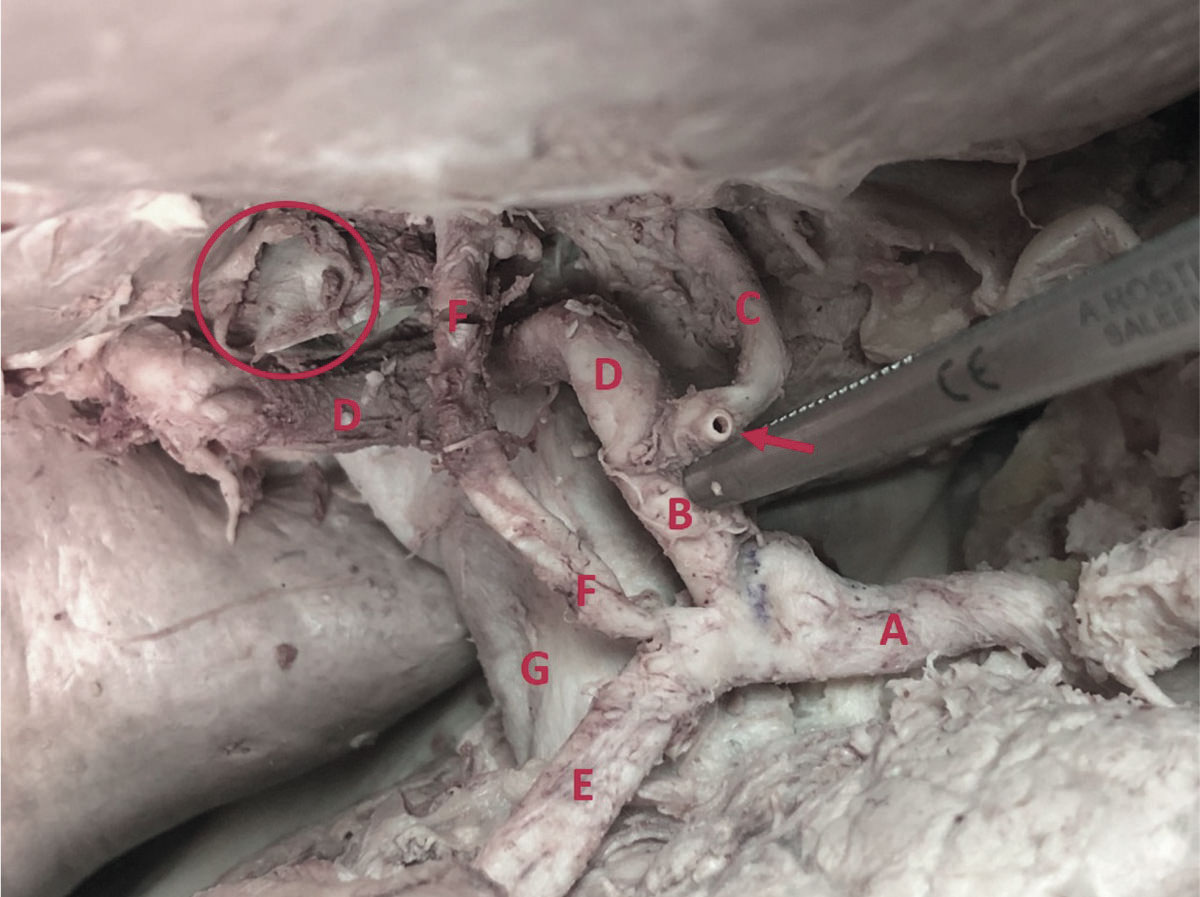
Here we present an anatomical variation of liver vascularization found during anatomical dissection. The variation was recognized upon opening the abdominal cavity and while dissecting porta hepatis. We found the celiac trunk originating from the abdominal aorta and branching normally into splenic, left gastric and common hepatic artery. Then, after arising from the celiac trunk, the common hepatic artery gave origin to its branch, the gastroduodenal artery. After branching of the gastroduodenal artery, the common hepatic artery ran further as the proper hepatic artery and finally split into the left and right hepatic artery, providing standard vascularization pattern with cystic artery arising from the right hepatic artery in the cystohepatic triangle (Caloti). While the course of the gastroduodenal artery was followed, its additional branch was noticed. The artery was parallel to the proper hepatic artery, medial to the common hepatic duct, superficial to the right hepatic artery, and at the level of the left hepatic artery. The artery entered porta hepatis between the right and left hepatic artery, just medial to the common hepatic duct. The accessory artery branched 6 mm after the gastroduodenal artery rose from the common hepatic artery. The length of the described accessory artery was 33 mm, with a diameter of 3.5 mm. The diameter of the left hepatic artery was approximately the same as the accessory artery (4 mm), while the diameter of the right hepatic artery was significantly larger (6 mm).
Considering the course of the accessory artery and the fact that it enters porta hepatis separately, not following the left or right hepatic artery, we can assume it provides arterial supply for the region defined as segments IVa and IVb (according to Couinaud’s liver segment classification).
COMMENTS
In 1966, Nicholas A. Michels established the classification of variants of hepatic arterial supply dividing it into ten types (Michels, 1966). Type I (Normal anatomy), II (left hepatic artery branching from a left gastric artery), III (right hepatic artery branching from a superior mesenteric artery) and IV (right hepatic artery arising from the superior mesenteric artery associated with the left hepatic artery arising from the left gastric artery) are most frequently found, according to Michels’ observations. Other variants of hepatic arterial supply, including the presence of accessory hepatic arteries or various combinations (type V – X) are less frequent (Fonseca-Neto et al., 2017). Later, in 1994, Jonathan R. Hiatt proposed another classification as an add-on to Michel’s systematization. Hiatt reduced Michels’ original ten groups to five most commonly found types, and introduced a sixth type of variation not previously described. In Hiatt’s version, type 1 resembles a classic pattern, type 2 replaced or accessory left hepatic artery from the left gastric artery, and type 3 replaced or accessory right hepatic artery from the superior mesenteric artery. All the double replaced patterns are put together in the type 4 group. The common hepatic artery arising from the superior mesenteric artery is defined as type 5 or type 6 if branching directly from the abdominal aorta (Hiatt et al., 1994). The last case can also be considered as type 2b variation of celiac trunk vascularization according to Marco-Clement et al. (2016) classification. However, some reports demonstrate that not all variations are included in the existing classifications. One of the most substantial reports regarding hepatic artery variations performed by Gruttadauria et al. (2001) showed that more than 6% of variations are not covered by present systematization.
Gruttadauria et al. (2001) found, among other variations, replaced right hepatic artery originating from the renal artery, replaced right hepatic artery originating from the left gastric artery and the right hepatic artery from the gastroduodenal artery. Koops et al. (2004) in their study described a case of a replaced right hepatic artery branching directly from the abdominal aorta, whereas Löschner et al. (2015) reported an accessory right hepatic artery arising directly from the abdominal aorta. Winston et al. (2007) in his publication reported a case of the replaced right hepatic artery from gastroduodenal artery, as well as a single case of the accessory artery for segment IV originating from the gastroduodenal artery, whereas Polguj et al. (2014) and Yamashita et al. (2015) described an accessory right hepatic artery arising from the gastroduodenal artery.
The embryological development of the liver might be a possible explanation for vascular variations of liver arterial supply. In early gestation life, the liver is supplied from three primary sources: the left hepatic artery from the left gastric artery, the middle hepatic artery, or common hepatic artery from the celiac trunk and the right hepatic artery from the superior mesenteric artery. During development, both right and left fetal hepatic artery should obliterate, leaving the whole liver vascularized by the middle hepatic artery (future common hepatic artery). In the case of partial or complete persistence of the fetal vascular pattern, anatomical variations may occur (Polguj et al., 2014; Noussios et al., 2017)
The clinical significance of accessory hepatic artery lies in surgical procedures involving the pancreatic head, bile duct, and liver. Pancreaticoduodenectomy (Whipple’s procedure) is a surgical procedure indicated in tumors of the pancreatic head, ampulla, and distal bile duct. Sometimes it can be performed in duodenal resection and chronic pancreatitis (Karim et al., 2018). During pancreaticoduodenectomy, the gastroduodenal artery is ligated just distal to its take-off from the proper hepatic artery. In the case of an existing accessory hepatic artery arising from the gastroduodenal artery, ligating proximally to the branching of the accessory hepatic artery may result in necrosis of the liver or bile ducts. However, it should be kept in mind that in case of malignant neoplasm of the pancreatic head, due to the preservation of the accessory hepatic artery, complete cancer resection may be compromised (Madhu and Harish, 2013; Chawla et al., 2018). Additional care should be taken in case of hepatoduodenal ligament resection. In liver transplantation, knowing the exact arterial vascularization of the liver is crucial in preserving complete blood supply to the graft or both grafts in case of split liver transplantation (Madhu and Harish, 2013). Furthermore, knowing exact vasculobiliary configuration in LDLT (living donor liver transplantation) is mandatory in order to prevent injuries and complications both in the liver graft and in the remaining donor liver (Kishi et al., 2010). Interestingly enough, Fouzas et al. (2019) reported in their study the increased incidence of early hepatic artery thrombosis in grafts with anatomic variations. Taking all of the stated into consideration, preoperative imaging of liver blood supply is mandatory in order to minimize complications during and after the operative procedure (Winston et al., 2007).
A limitation of our presumption is that we do not have any imaging or clinical proof of the significance of our accessory artery. Even though this finding may have a strong clinical impact, in order to determine its true relevance additional clinical test and research should be done.
Conclusion
Having in mind that numerous anatomical variations, not included in any of existing classifications, could be present, it is crucial to be familiar with those deviations while performing surgical procedures including hepatobiliary system, pancreas, and duodenum. The presented case of the accessory artery might be significant in clinical settings due to its impact on intra- and postoperative outcomes.
Acknowledgements
The authors would like to thank the body donor for his selfless gift for the benefit of science and medical education. We would also like to thank all the members of Department of Anatomy and Clinical Anatomy, School of Medicine, University of Zagreb and Division of Abdominal Surgery and Organ Transplatation, Department of Surgery, University Hospital Merkur, Zagreb for their kind cooperation and help. The authors thank Krunoslav Užarević, PhD, Ruđer Bošković Institute, Zagreb and Mia Vrbanac Užarević for their comments and suggestions.
Related articles
CHAWLA A, ROSENTHAL MH, CLANCY TE (2018) Implications of the replaced right hepatic artery originating from the gastroduodenal artery in the setting of a pancreatic head mass. Clin Imag, 52: 189-192.
FONSECA-NETO OCL da, DE SOUZA LIMA HC, RABELO P, VIEIRA DE MELO PS, AMORIM AG, MOURA LACERDA C (2017) Anatomic variations of hepatic artery: a study in 479 liver transplantations. Arq Bras Cir Dig, 30(1): 35-37.
FOUZAS I, PAPANIKOLAOU C, KATSANOS G, ANTONIADIS N, SALVERIDIS N, KARAKASI K, VASILEIADOU S, FOUZA A, MOULOUDI E, IMVRIOS G, PAPANIKOLAOU V (2019) Hepatic artery anatomic variations and reconstruction in liver grafts procured in Greece: the effect on hepatic artery thrombosis. Transplant Proc, 51(2): 416-420.
GRUTTADAURIA S, FOGLIENI CS, DORIA C, LUCA A, LAURO A, MARINO IR (2001) The hepatic artery in liver transplantation and surgery: Vascular anomalies in 701 cases. Clin Transplant, 15(5): 359-363.
HIATT JR, GABBAY J, BUSUTTIL RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg, 220(1): 50-52.
KARIM SAM, ABDULLA KS, ABDULKARIM QH, RAHIM FH (2018) The outcomes and complications of pancreaticoduodenectomy (Whipple procedure): Cross sectional study. Int J Surg, 52: 383-387.
KISHI Y, IMAMURA H, SUGAWARA Y, SANO K, KANEKO J, KOKUDO N, MAKUUCHI M (2010) Evaluation of donor vasculobiliary anatomic variations in liver graft procurements. Surgery, 147(1): 30-39.
KOOPS A, WOJCIECHOWSKI B, BROERING DC, ADAM G, KRUPSKI-BERDIEN G (2004) Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg Radiol Anat, 26(3): 239-244.
LÖSCHNER C, NAGEL SN, KAUSCHE S, TEICHGRÄBER U (2015) Hepatic arterial supply in 1297 CT-angiographies. RoFo (Fortschritte auf dem Gebiet der Rontgenstrahlen und der Nuklearmedizin), 187(4): 276-282.
MADHU YC, HARISH K (2013) Accessory right hepatic artery and its implications for a surgeon. Ind J Surg, 75(1 suppl.): 492-494.
MARCO-CLEMENT I, MARTINEZ-BARCO A, AHUMADA N, SIMON C, VALDERRAMA JM, SANUDO J, ARRAZOLA J (2016) Anatomical variations of the celiac trunk: cadaveric and radiological study. Surg Radiol Anat, 38(4): 501-510.
MICHELS, NA (1966) Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg, 112(3): 337-347.
NOUSSIOS G, DIMITRIOU I, CHATZIS I, KATSOURAKIS A (2017) The main anatomic variations of the hepatic artery and their importance in surgical practice: review of the literature. J Clin Med Res, 9(4): 248-252.
POLGUJ M, PODGÓRSKI M, HOGENDORF P, TOPOL M (2014) Variations of the hepatobiliary vasculature including coexistence of accessory right hepatic artery with unusually arising double cystic arteries: Case report and literature review. Anat Sci Int, 89(3): 195-198.
WINSTON CB, LEE NA, JARNAGIN WR, TEITCHER J, DEMATTEO RP, FONG Y, BLUMGART LH (2007) CT angiography for delineation of celiac and superior mesenteric artery variants in patients undergoing hepatobiliary and pancreatic surgery. Am J Roentgenol, 189(1): W13-9.
YAMASHITA K, HASHIMOTO D, ITOYAMA R, OKABE H, CHIKAMOTO A, BEPPU T, BABA H (2015) Accessory right hepatic artery branched from gastroduodenal artery. Surg Case Rep, 1: 90.