INTRODUCTION
Ponticulus posticus (PP) is an anatomical variation from the first cervical vertebra (Atlas) in which a bony bridge joins the lateral mass to the posterior arch: it has been an object of study and included in photographic atlas (Mann et al., 2016). This definition corresponds to the complete ponticulus posticus, being more frequent to find an incomplete bridge.
Its prevalence varies between the populations under study or according to the study method that is employed, having an incidence range from 1% to 46%, according to different authors (Bayrakdar et al., 2018; Donald et al., 2017; Giri et al., 2017; Lo Giudice et al., 2018).
The authors present a study about the presence of the ponticulus posticus in dry bone pieces and imaging studies.
MATERIALS AND METHODS
A total of 77 dry bone pieces from Facultad de Medicina, Universidad de la República (Montevideo, Uruguay) and UCLAEH (Maldonado, Uruguay) were examined. In these, the presence of the PP was searched macroscopically registering whether it was present or not. If present, its corresponding side of appearance, and whether it was complete or incomplete. Other variations of the atlas were also registered. To reduce the inter observer bias, the 77 dry bone pieces were evaluated by the same examiner.
Simultaneously, 55 computed tomography (CT) multi detector of normal cervical spine were collected randomly, including the totality of the cervico-occipital junction. The obtained images were reprocessed with the Volume Rendering (VR) protocol for the study of the 3D images in different approaches, and were reviewed by a radiology physician with expertise. The age and gender of the patients were registered. In these CT images, presence of PP, side, and complete/incomplete status were also assessed.
In the identification of the PP, we adopted the classification applied by Lo Giudice, which defines complete PP when a full osseous ring was formed above the posterior arch, and incomplete PP when the extension of the bridge was larger than half the distance between the posterior arch and the articular process of the atlas (Lo Giudice et al., 2018). This author only applied this to imaging studies, while we applied this to the 55 imaging studies and the macroscopic analysis of the 77 pieces.
Data were registered in Microsoft Office Excel, and Chi-square test and Z-test for proportion comparisons were used to identify associations and differences between variables. A p-value under 0.05 was considered statistically significant.
RESULTS
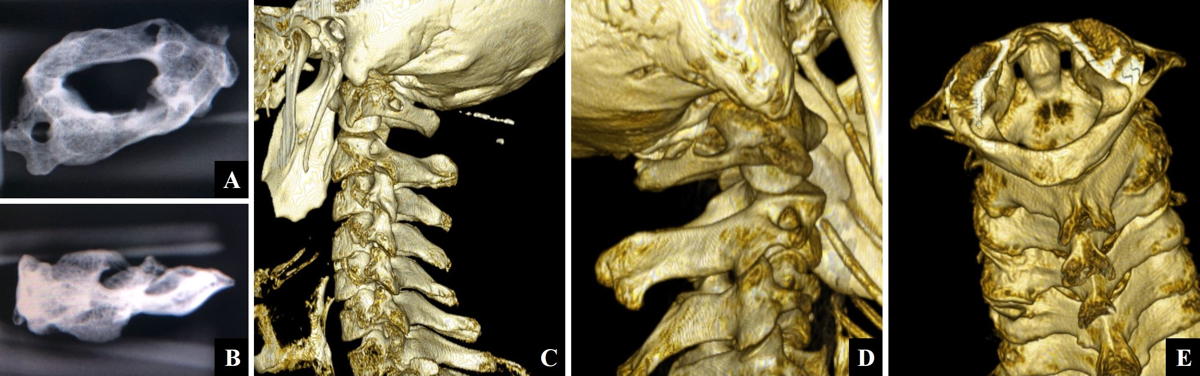
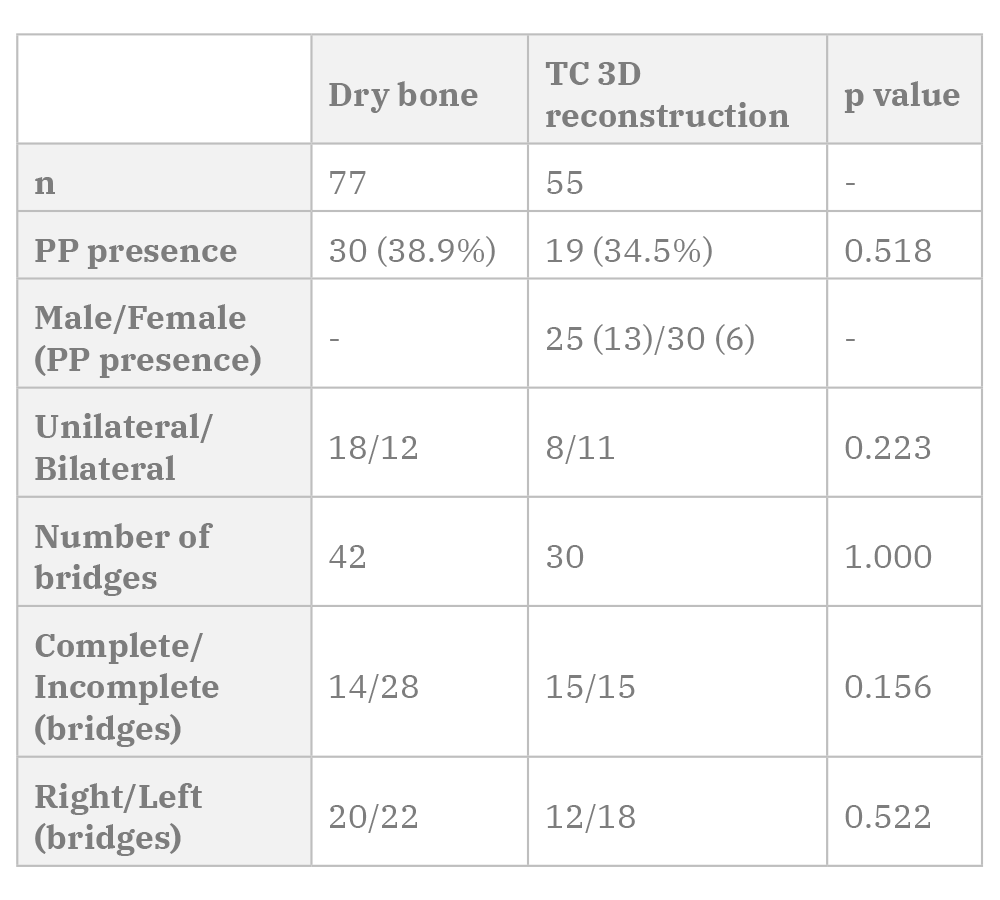
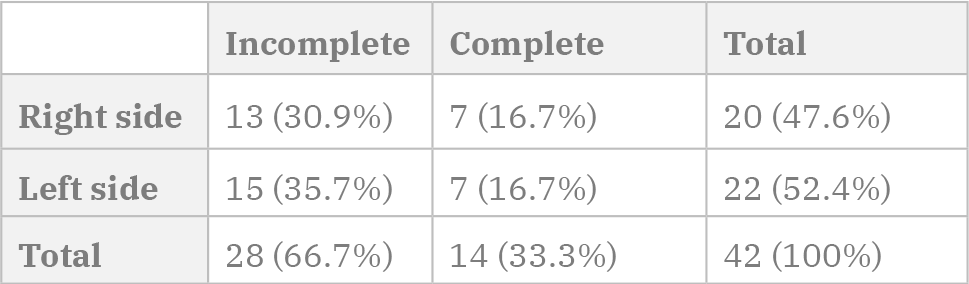
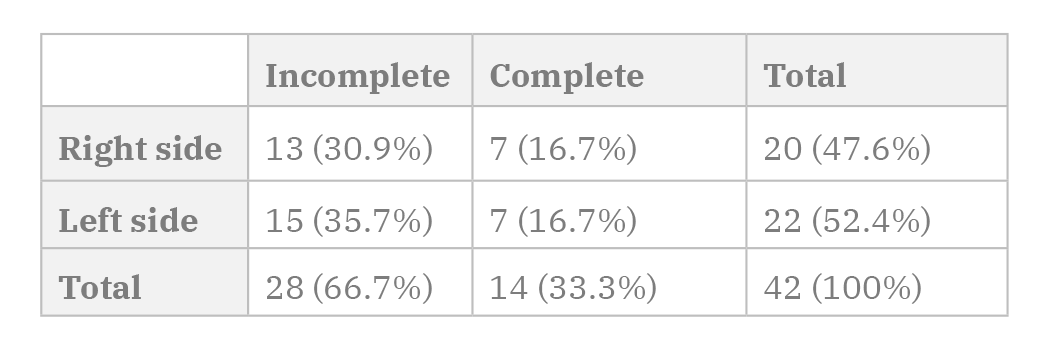
Out of the 77 analyzed dry bone pieces, 30 presented bony bridges (38.9% of the pieces). The corresponding data is shown in Table 1 and few examples appear in Fig. 1.
Twelve atlases presented bilateral bony bridges (15.6% of the total, 40.0% of the vertebrae with bridges) while 18 presented unilateral bridges (23.4% of the total, 60.0% of the vertebrae with bridges).
Because of this, a total of 42 bridges were accounted, whether they were complete (14 bridges, 33.3% of the pieces with PP) or incomplete (28 cases, 66.7% of the pieces with PP).
The side of the bony bridges and the presence of a complete or incomplete bridge did not show a statistically significant association (p=0.827) (Table 2).
The sole other variation found was the presence of 3 pieces with absence of laminar fusion in the posterior middle line. Of these 3 pieces, 1 presented bilateral incomplete bridges (Fig. 1E), 1 presented bilateral complete bridges (Fig. 1F) and 1 presented no bony bridges.
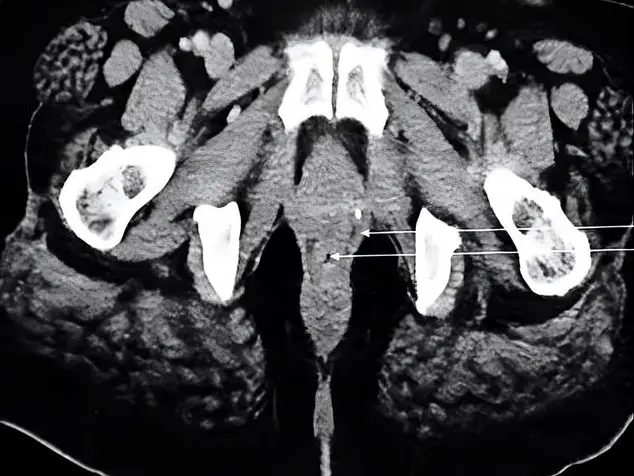
Regarding the analysis of the 3D CT images (Table 1) (Fig. 2), studies from both genders were analyzed (25 male and 30 female), ages ranged between 16 and 83 years, with a mean of 49 years. Nineteen pieces presented bony bridges (34.5% of the analyzed images) from which 11 were bilateral cases (20.0% of the total, 57.9% of the vertebrae with bridges) and 8 were unilateral cases (14.6% of the total, 42.1% of the vertebrae with bridges). This totalize 30 ponticulus posticus, 12 were located on the right side and 18 on the left side (no statistically significant difference). A total of 15 complete and 15 incomplete PP were found.
Out of the 25 men, 13 presented bony bridges (52.0%), while in the 30 women only 6 presented PP (20.0%). A statistically significant association was found between the presence and male gender (p=0.013) (Table 3).
When we compare the PP prevalence between the dry bone material and imaging studies, 38.9% and 34.6% were the obtained values respectively, with no statistically significant difference.
Finally, no statistically significant differences were found when comparing the proportions for number of bridges, bilateral or unilateral bridges, and complete or incomplete bridges between the dry bone material and the imaging studies (Table 1).
DISCUSSION
The presence of bony bridges in the posterior sector of the atlas has called the attention of investigators and physicians due to its potential association with many pathologic states.
The ponticulus posticus is a bony bridge, complete or incomplete, extended from the posterior aspect of the articular process of the atlas to its posterior arch. Although it is sometimes considered an “anomaly”, it is relatively frequent, being found in up to 46% of the cases (Giri et al., 2017), and most of the times it may not be discovered since it could not produce pathology. Three or four variants of the PP are described, depending of the consulted author.
Miki et al. state 3 variants: complete bridge, incomplete bridge or calcification. The latter is a bony spicule that raises from the lateral mass. In our pieces, we only consigned whether the bridge was complete or incomplete, as we believe there is no major clinical impact in discriminating the calcification from the incomplete bridge (Donald et al., 2017).
A lateral bridge extended from the lateral mass to the transverse process may be found, among other common variations, such as an accessory foramina. These findings should be differentiated from the PP (Mann et al., 2016).
The prevalence of PP is very variable according to the study method. This one can vary from the review of skeletal material, the dissection of fresh or fixated corpse material and the utilization of imaging studies, such as radiographies, computed tomography or magnetic resonance images (Hauser and De Stefano, 1989). Likewise, the variations could be due to the population under study, as it may be linked to their genetic background (Bayrakdar et al., 2018). As far as we are concerned, there is no previous study of prevalence of the PP in Uruguayan population. The frequency of PP in our bone pieces and in the imaging studies (38.9% and 34.6%, respectively) shows no statistical difference between these two resources, and rate among the highest incidences reported. According to Baraykdar et al. (2018) the PP is more frequent in European and North American populations than the ones reported from Asian populations and it is more frequent in males than females. The Uruguayan population is constituted from the ethnic point of view, by more than 85% of European descendants, around 10% of Afro-American population, and approximately 5% that manifests having indigenous descent (Klüver et al., 2019). Taking this into account, it is not striking that our results are comparable to those of European population. In a regional study from Peru, 1056 lateral cephalograms of Peruvian population were reviewed and an incidence of 19.8% of the PP was observed (Pérez et al., 2014). This incidence differs significatively from our results (p-value < 0,001) and could be explained because of a different ethnic constitution of the Peruvian population.
In our series of bone pieces, we could not determine the gender of the analyzed atlases, but in the imaging series gender was assessed. We found that men have a higher incidence of PP and that this association is statistically significant. This is consistent with authors such as Baraykdar et al. (2018). Arslan et al. (2018) observed the opposite, finding a higher incidence in female gender unlike our series; this author could also register a greater incidence of the PP in the right side, both these results with statistically significant difference.
About the unilaterality/bilaterality, the reports are dissimilar. In fact, our study showed greater unilateral proportion in the dry bone pieces while the CT analysis showed greater bilateral proportion (with no significant difference). Series presented by Tripodi et al. (2019) reported that 74,3% of the bridges were bilateral. A study including 181 patients showed results more similar to our TC analysis: 43.9% of patients with unilateral bridges against 56.1% of bilateral bridges (Bayrakdar et al., 2018).
In the consulted literature, the presence of complete bridges ranges between 0.9% and 18%. Predominantly, the series show a higher frequency of incomplete bridges than complete bridges (Bayrakdar et al., 2018; Giri et al., 2017; Tripodi et al., 2019). Our general results are comparable to the majority of the consulted literature, and we also found higher rates of incomplete PP in our bone pieces.
Regarding the origin of PP, it is not clear, and several theories have been presumed. The most discussed ones describe the PP as the result of post traumatic exposure, as a variation appeared due to evolutionary or genetic factors, or as the ossification of the occipito-atlantoid ligament, these being considered normal ontogenetic processes (Bayrakdar et al., 2018). About the latter, the relatively high incidence in pediatric population is against it. Tripodi et al. (2019), having analyzed 524 CT scans from children up to 17 years old, founds complete and incomplete bony bridges in 28.2% of the cases. The ontogenetic theory due to aging and calcification of the ligament does not match with this incidence in the pediatric population.
Several clinical implications of the PP have been described in the bibliographic research. It has been associated with cervicogenic headache, tinnitus, migraine, vestibular symptoms, vertebrobasilar insufficiency, photophobia, eye pain, brachialgia, omalgia, oculomotor disorders, diplopia, strokes or even dysphagia and hearing loss (Arslan et al., 2018; Bayrakdar et al., 2018; Donald et al., 2017; Giri et al., 2017; Tripodi et al., 2019). Having its location into account, its relationships, and the incidence of PP in populations of all ages, the authors of this study believe it to be unlikely that all these clinical manifestations can be related to the PP. Nevertheless, it does have clinical and surgical implications in some scenarios.
When there is a complete PP, it forms an osseous ring in which the vertebral artery and the first spinal nerve can be found. So, anatomically, it is difficult to explain oculomotor disorders, dysphagia or vestibular symptoms if not by an ischemic mechanism or a diminishment of blood flow to the nucleus, via, or cranial nerves implicated in those functions. If we suppose that due to the PP the blood flow has been compromised, then the other vertebral artery could supply (Prinzo et al., 2006). Thus, it seems unlikely that the PP is responsible for these symptoms, especially having into consideration its high incidence in general population.
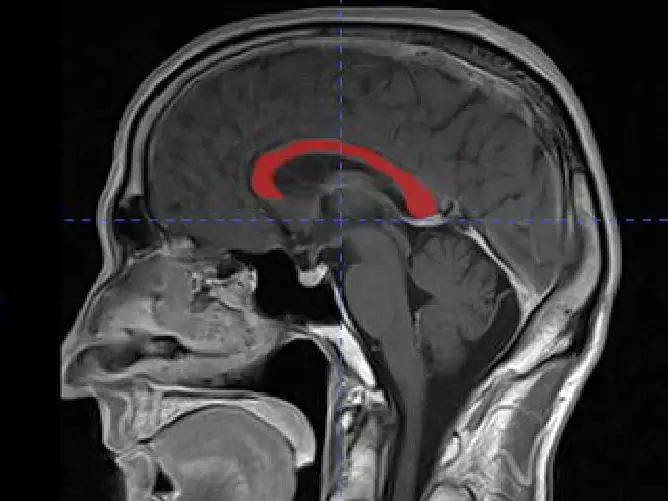
Another scenario in which it is of interest to know in advance the presence of the PP is in the surgery of tumoral injuries of the occipito-atlantoid region (Fig. 3). In some of these injuries, it can be necessary to move the vertebral artery during the procedure, or even the tumor itself can displace the vertebral artery, as it is shown in Fig. 3, where the expansive process (schwannoma of C1) has displaced the vertebral artery upwards and laterally. The presence of a bony bridge modifies the surgical strategies since the surgeon could angle the artery against the bridge and decrease its blood flow.
In a local study about the configuration of the posterior sector of the cerebral arterial circle, 35 adult encephala were dissected. In this sector, a 57.1% of variations were registered. We highlight that the caliber of the left vertebral artery was larger in 45% of the cases, 50% the calibers where similar and only in 5%, the caliber of the right vertebral artery was larger (Martínez et al., 2003) These considerations are essential along with the consideration of the PP. If for example, the schwannoma compresses the left vertebral artery against the PP, and this artery is responsible for the vast blood flow of the posterior fossa, the right vertebral artery may not me capable to supply in case of having a small caliber.
In case of occipito-atlantoid instability, it may be necessary to collocate a fixation system with screws and bars. In the presence of PP, during the intra operatory procedure, the surgeon can misinterpret that he is in front of a wide posterior arch, and collocate a screw through the bony bridge, with the risk of injuring the vertebral artery and first cervical nerve (Sharma et al., 2010). Song et al. investigated the impact of present PP in two high cervical surgeries (arthrodesis of posterior arch to lateral mass and occipito-condylar arthrodesis), both with screws. They concluded that both techniques were feasible and secure in presence of PP, and even stated that when increasing the distance between the vertebral artery and the occipital, in the case of occipito-condylear fixation, the presence of the PP could mean an anatomic advantage in this procedure. Nevertheless, in female patients such dimensions are smaller and surgeon should be cautious, according to the investigators (Song et al., 2017). Findings by Arslan et al. (2018) suggest that the presence of the PP does not alter the feasibility and security of lateral mass fixation; contrarily, these researchers state that this bony bridge is associated with narrower vertebral arteries. These are some of the reasons why it is handy to know in advance the presence of the PP, especially to identify it before surgical procedures.
Zhang et al. (2016) carried out a retrospective study about screw fixation in patients with atlantoaxial instability. They included 28 patients with atlas variations, which they defined in three groups depending on the height of the arterial groove and height of the posterior arch, being these groups of interest because this fixation technique is not suggested when any of these measures <4,0 mm, since these reduced distances could increase the difficulty of the procedure of fixation. The presence of a bony bridge in the posterior arch should be taken into account, as it may lead to misinterpretation of its height, and therefore surgical planning would have the wrong anatomical bases with the consequent wrong surgical procedure.
Conclusions
Ponticulus posticus is a high prevalence variation, that usually goes unnoticed if its systematic research is not carried out. Our results rate among the higher prevalence reported. Clinical and surgical implications justify why knowing its presence is of great interest either as a numerous medical condition-associated variation, or as a condition to take into account in surgery planification.
Acknowledgements
The authors express their recognition to all who, in life, decide to donate their body to our Faculty, for teaching and research of Anatomy.