The processus vaginalis (PV) is an embryonic diverticulum of the parietal peritoneum at the deep inguinal ring. The patent processus vaginalis (PPV) is the etiology for the development of an indirect inguinal hernia, and is associated with undescended testis, scrotal hydrocele. The aim of this study was to examine the characteristics of PPV in Vietnamese patients: a total of 309 adult patients who underwent transperitoneal laparoscopic surgery (TPLS) from March 2019 to March 2020 at Hue University of Medicine and Pharmacy Hospital. When a PPV was identified, the side and the size of PPV was recorded. Statistical analysis was done using the p-Value test for strength of evidence. The incidence of PPV of 309 subjects was 22 cases (7.1%). The rate of PPV in males was 12.1% and 3.0% in females (p = 0.002). The rate on the right side was 4.5%, 1.9% on the left and 0.7% on both sides. The mean PPV size was 6.1 mm ± 4.1 mm and 3.0 mm ± 0.7 mm in males and females, respectively (p = 0.004). Of all patients (both male and female) that had PPV, 3 patients (4.7%) had a BMI ≥ 23 and 19 patients (7.3%) had a BMI <23. Knowledge of the anatomy and embryology of PV and the mechanisms of obliteration and PPV can assist clinicians and ultrasonographers in the evaluation and treatment of patients who present with asymptomatic PPV.
Patent processus vaginalis in Vietnamese adults who underwent laparoscopic transperitoneal surgery
Tri Huu Nguyen1A, Tung Sanh Nguyen1A, Vung Phuoc Doan2A, Hoang Nguyen1A, Bao Hoai Vo1A, Phuc Thanh Nguyen1A, Luu Ba Nguyen1A, Thao Minh Nguyen1A, Ernest F. Talarico, Jr.3B
1 Department of Anatomy and Surgical Training
2 Department of Digestive Surgery
3 Department of Anatomy
A Hue University of Medicine and Pharmacy, Hue University, Hue city, Việt Nam
B Tan Tao University School of Medicine, Long An Province, Việt Nam
SUMMARY
Sign up or Login
ABBREVIATIONS
Body Mass Index (BMI)
Computed Tomography (CT)
Laparoscopic Transperitoneal Surgery (LTPS)
Patent Processus Vaginalis (PPV)
Perforated Duodenal Ulcer (PDU)
Processus Vaginalis (PV)
Tunica Vaginalis (TV)
INTRODUCTION
The processus vaginalis (PV) is an embryonic diverticulum (i.e., blind ended-pouch) of the parietal peritoneum at the deep inguinal ring, growing into the mesenchyme of the gubernaculum, inguinal canal and the scrotum. The PV begins forming in the 8th week of embryogenesis in both males and females (Godbole et al., 2010). In males it is linked to testicular descent down within the gubernaculum (Bouzada et al., 2017), and is found in all species where the male gonad descends through the inguinal canal (Godbole et al., 2010; Brainwood et al., 2020). Although the mechanism of its role in testicular descent remains unclear, it has been suggested that the PV dilates the pathway for testicular descent through the inguinal canal and into the scrotum (Burgu et al., 2010). PV closure (i.e., fusion) occurs at any point from a few weeks before birth (i.e., prenatally), to a few weeks after birth (i.e., postnatally) (Clarnette and Hutson, 1999; Brainwood, et al., 2020). The remaining portion around the testes becomes the tunica vaginalis (Clarnette and Hutson, 1999). In females, if the PV does not close, it forms the Canal of Nuck, an open pouch of peritoneum extending into the labia majora. It is more rudimentary than in males (Sameshima et al., 2017; Laing et al., 2007). The Canal of Nuck accompanies the gubernaculum, which differentiates to become the round ligament of the uterus (Clarnette and Hutson, 1999; Sameshima et al., 2017; Laing et al., 2007). It has been suggested that it assists the gubernaculum in the normal anteverted, anteflexed positioning of the uterus, and in preventing ovarian descent into the inguinal canal (Rees et al., 2017; Holley, 2018).
There are many theories regarding the timing of PV closure. In normal development, the PV with the exception of the TV (in males) is obliterated prenatally or early in life (Clarnette and Hutson, 1999; Mitchell, 1939; Hata et al., 2004; Van Veen et al., 2007, Moore et al., 2011). Prior studies show that prenatal obliteration occurs in 80% of males and 60% of females (Favorito et al, 2005; Rahman et al., 2009). At 8 weeks of age, 63% of male neonates may have a patent processus vaginalis (PPV) with closure or obliteration occurring up until the age of 2 years (Van Veen et al., 2007). While the incidence of PPV has been suggested to decrease after one year of age and to plateau by 3-5 years of age (Clarnette and Hutson, 1999), more recent studies have documented that 40% of males continue to have PPV and half are asymptomatic throughout life (Van Veen et al., 2007; Favorito et al., 2009). PPV in children has been studied by many authors. Weaver et al. (Weaver et al., 2016) indicated that the prevalence of the asymptomatic PPV in children who underwent laparoscopic surgery was approximately 20%.
When obliteration fails, a wide variety of conditions associated with PPV may occur (Wessem et al., 2003; Van Veen et al., 2007; Abrahamson, 1998). These conditions include indirect inguinal hernias in children and in adults, as well as hydroceles and undescended testes (Van Wessem et al., 2003; Van Veen et al., 2007; Abrahamson, 1998; Rafailidis et al., 2016; Dagur et al., 2017; Rees et al., 2017; Godbole et al., 2010, Han et al., 2002). Because cryptorchidism (i.e., undescended testes) is a risk factor in testicular cancers, PPV may also have a role in the genesis of male gonadal cancers (Talarico, Jr., et al., 2018).
A survey of the literature shows that the incidence of PPV and resulting medical conditions have not been documented in Vietnam. Although a potential association between testicular cancer in dogs and their service in Vietnam following exposure to Agent Orange has been shown (Hayes et al, 1990; Hayes et al., 1991; Hayes et al. 1995; NASEM, 2018), it is not clear that this is related to PPV or data of testicular cancers in humans. Currently, laparoscopic transperitoneal surgery (LTPS) done for different medical conditions allows surgeons to efficiently investigate the deep inguinal ring, and results in identification of PPV in patients who underwent the LTPS. In the present study, LTPS is used for examining the characteristics of PPV in the adult Vietnamese population.
MATERIALS AND METHODS
Subject Cohort
Prior to the beginning of this study and subject recruitment, approval was obtained from the Internal Review Board of Hue University of Medicine and Pharmacy Hospital, a single tertiary care hospital. Patient consent was obtained. The benefit(s) to patients for participation in this study were none, and patient care/treatment was not affected by enrolment in, or exclusion from, this research investigation.
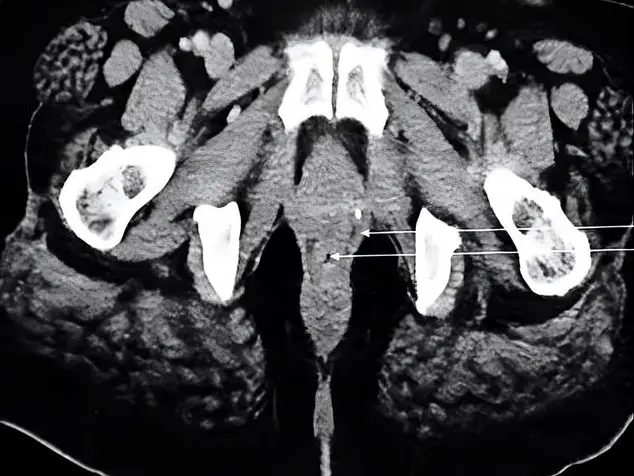
A total of 309 adult patients (141 males and 168 females), who underwent LTPS from March 2019 to March 2020, were enrolled in this study. All subjects in this study were given thorough physical examinations, and each had ultrasound examination to rule out the presence of asymptomatic inguinal hernia. Only in the case of patients with colon cancer, preoperative abdominal computed tomography (CT) was done. Subjects were excluded from this cohort if they (1) had multiple adhesions at the deep inguinal ring that prevented the surgeon from observation, (2) had symptoms of inguinal hernia, or (3) had prior hernia repair. The age range of subjects was 17 to 90 years with a mean age of 43.2 years. Body Mass Index (BMI) ranged from 13 to 32 kg/m2, with a mean BMI of 21.0 kg/m2. The reasons for LTPS were appendectomy, cholecystectomy, colectomy or perforated duodenal ulcer (PDU). The majority of patients (91.9%) underwent laparoscopic appendectomy. These demographics are summarized in Table 1.
Table 1. Patient Demographics.
|
Variables |
Value (n=309) |
|
Age (years) (min - max) |
43.2 ± 17.0a (17-90) |
|
Sex, no. (%) Male Female |
141 male (45.6) 168 female (54.3) |
|
BMI (kg/m2) (min - max) |
21.0 ± 2.7a (13-32) |
|
Reasons for LTPS Appendectomy, no. (%) Cholecystectomy, no. (%) Colectomy, no. (%) Others (PDU,..), no. (%) |
284 (91.9) 13 (4.2) 9 (2,9) 3 (1.0) |
a Value is mean ± standard deviation.
Laparoscopic Transperitoneal Surgery (LTPS)
Perforated Duodenal Ulcer (PDU)
LTPS Procedure and Measurements
Patients were placed in the Trendelenburg position at a 30º angle for inspection of both sides of the deep inguinal ring. A 30º telescope was used to visualize the deep inguinal ring region. The deep inguinal ring is the site where the vas deferens and the testicular vessels join to pass through the abdominal wall in males. In female, the round ligament was used for identifying the deep inguinal ring. A PPV was identified as a peritoneal protrusion at the deep inguinal ring site. When a PPV was found, the side and the size of PPV were recorded. The size of PPV was measured in comparison with the 5 mm tip of the suction-irrigation tube. All metric data were tabulated in Microsoft Excel 2016 (Microsoft®, Redmond, Washington, USA), and statistical analysis was done using the p-Value test for strength of evidence.
RESULTS
PPV Characteristics
The incidence of PPV of 309 subjects was 22 cases (7.1%). Of these cases, 17 were males (12.1%; Table 2 and Fig. 1) and 5 females (3.0%; Table 2 and Fig. 2). Overall, 14 (4.5%) were right-sided and 6 (1.9%) were left-sided (p = 0.002). In only 2 cases (0.7%), bilateral PPV was discovered. For all subjects, the mean size of the PPV was 5.6 mm; with a range of 2 mm - 15 mm. The mean PPV size was 6.1 mm ± 4.1 mm and 3.0 mm ± 0.7 mm in males and females, respectively (p = 0.004). The PPV characteristics of this cohort are summarized in the Table 2.
Table 2. Characteristics of Patent Processus Vaginalis discovered during laparoscopic procedures.
|
PPV CHARACTERISTICS |
VALUE |
P VALUE |
|
PPV no. (%) |
22 (7.1) |
|
|
Sex, no. (%) Male, no. (%) Female, no. (%) |
17 (12.1) 5 (3.0) |
0.002 |
|
Location (side) Right side, no. (%) Left side, no. (%) Bilateral, no. (%) |
14 (4.5) 6 (1.9) 2 (0.7) |
0.002 |
|
Size of PPV (mm) (min - max) Male (mm) Female (mm) |
5.6 ± 3.9a (2 - 15) 6.1 ± 4.1a 3.0 ± 0.7a |
0.004 |
a Value is mean ± standard deviation
Patent Processus Vaginalis (PPV)
BMI and PPV
In Việt Nam, high BMI is defined as ≥ 23 (Thandassery et al., 2013; WHO, 2004). Generally, male subjects had higher BMIs than females. Of the subjects evaluated in this study, 102 (72.3%) of males and 143 (85.1%0 of females had a normal BMI, whereas 39 (27.7%) of males and 25 (14.9%) of females had an elevated BMI. Of all patients (both male and female) that had PPV, 3 patients (4.7%) had a BMI ≥ 23 and 19 patients (7.3%) had a BMI <23 (p = 0.395). These results are summarized in Table 3.
DISCUSSION
The PV is an embryonic protrusion of the parietal peritoneum at the deep inguinal ring. Normally, the PV is obliterated, except for the distal part covering for the testes persisting as the tunica vaginalis (Clarnette and Hutson, 1999). PPV is associated with various pathological conditions, including congenital indirect inguinal hernias and hernias in adults (Clarnette and Hutson, 1999; Van Wessman et al., 2003; Van Veen et al., 2007; Brainwood et al., 2020), and scrotal hydroceles and encrusted hydroceles of the cord (Brainwood et al., 2020). Many investigations suggest a strong relationship between PPV and cryptorchidism (Favorito et al., 2005; Cives et al., 1996; Lee et al., 2015). Secondarily, due to the association between cryptorchidism and testicular cancers, PPV may also be related to seminomas and non-seminoma cancers (Talarico et al., 2018).
The mechanism(s) of PV closure are not understood, but seem to involve apoptosis of smooth muscle cells within the PV (Mouravas et al., 2010; Hosgor et al., 2004). Currently, it is thought that obliteration occurs in three stages (I, II and III) in males in contrast to two stages in females (Rafailidis et al., 2016; Rees et al., 2017; Brainwood et al., 2020). Stage I is proximal closure of the deep inguinal ring sealing off the PV from the peritoneum (Rafailidis et al., 2016). Stage I occurs in both males and females. Stage II in males is the distal closure of the PV superior to the testis. Stage III is atresia of the funicular process (i.e., the remaining tube-like structure between these two proximal and distal points of closure) (Brainwood et al., 2020; Singh et al., 2010). However, the distalmost portion of the PV remains forming the TV. In contrast, Stage II (the final stage) in females is the atresia of the Canal of Nuck (Rees et al., 2017). Failure of closure can occur at any stage. However, when closure fails across all three stages, the PPV extends from the deep inguinal ring to the scrotum (or labia majora in females), and is thought to result in indirect inguinal hernias and hydroceles (Rafailidis et al., 2016). This communication may also allow the movement of pus or an infectious process into the scrotum or labia majora, as well as the implantation of endometriosis or zygotes at any location within the Canal of Nuck (Rahman et al., 2008; Okoshi et al., 2017; Shehzad and Riaz, 2011; Gaeta et al., 2010; Noguchi et al., 2014).
A survey of the published literature shows that most studies on PPV were conducted on children, and that PPV studies are quite rare in adults. Still further, no studies were found where the subject cohort was a Vietnamese population. In the present work, of 309 subjects examined only 22 (7.1%) had asymptomatic PPV (Table 2). The mean size of PPV was 5.6 ± 3.9 mm, and the mean size of PPV in males was higher than in females: 6.1 mm vs 3.0 mm (p = 0.004) (Table 2). These results are similar to those of Watson et al. (Watson et al, 1994) and Van Veen et al. (Van Veen et al., 2007), who reported rates of asymptomatic PPV in adults of 9.0% and 15.4%, respectively. Further, the presence of asymptomatic PPV in Vietnamese subjects did not correlate to age. This supports a study done by Van Veen et al. (Van Veen et al., 2007) that showed no significant correlation between age and the prevalence of PPV. In contrast, Weaver et al. (Weaver et al., 2016) examined 1548 infants and children who underwent a non-hernia-related TPLS and found the rate of asymptomatic PPV was 20%.
In this Vietnamese cohort, there was a significant difference between the rate of PPV (in adults) on the right and left sides: 4.5% vs 1.9% for the right side and left side, respectively (p = 0.002) (Table 2). Comparing these results to published studies, many authors reported a difference of PPV between prevalence on the right side and the left side. In one study, the rate of PPV in children was much higher on the right side (46%) in contrast to the left side (14%) (Weaver et al., 2016). It is suggested that one reason for this is that the left PV is obliterated earlier; therefore, the PPV prevalence is higher than on the left side (Clarnette and Hutson, 1999; Brainwood et al., 2020). From a clinical viewpoint, it is interesting to note that the incidence of a contralateral PPV in children who also had a unilateral inguinal hernia was very high. Rowe et al. (Rowe et al., 1969) studied 2764 patients ranging from 1 day to 16-years-old who underwent surgery for inguinal hernia, and showed that the rate of PPV on the side opposite the hernia was 63% in the first 2 months of life, and 41% in patients from the age of 2 to 16 years. George et al. (George et al., 1996) reported a similar rate of PPV on the side opposite of 41% in patients under 10 years of age.
There was a significant difference in the comparison between the rate of PPV in Vietnamese males and females, or 12.1% and 3.0%, respectively (p = 0.002). Prior studies done in different populations also show similar results. Watson et al. (Watson et al., 1994) reported the rate of PPV of 19% and 8% in American males and females, respectively. Of children born and living near Aberdeen, Scotland, the rate of PPV was 84.2% in males and 70% in females. (Mitchell, 1939). Van Veen et al. (Van Veen et al., 2007) demonstrated the incidence of PPV was 3.44 times higher in men born and living in the Netherlands (30.9% in men vs 9.5% in women).
PPV is the aetiology for the development of indirect inguinal hernia in children and in adult (Van Veen et al., 2007; Weaver et al., 2016). The higher incidence of PPV in men and on the right side might explain the reason why the indirect hernias in men and on the right side higher than in women and on the left side (Zhao et al., 2017). Rowe et al. (Rowe et al., 1969) reported that the prevalence of the inguinal hernia on the right, on the left and bilateral were 60%, 30%, 10% respectively. According to Van Veen et al. (Van Veen et al., 2007), the incidence of indirect inguinal hernias was five times higher in men.
BMI is a person’s weight in kilograms divided by the square of height in meters (kg/m2). A high BMI can be an indicator of high body fatness. BMI can be used to screen for weight categories that may lead to health problems, but it is not diagnostic of the body fatness or health of an individual. The results of the present research showed that in all subjects who had PPV, 3 patients (4.7%) had a BMI ≥ 23 and 19 patients (7.3%) hnd a BMI <23. Prior studies suggest that the incidence of primary inguinal hernia decreases as BMI increases (Zendejas et al., 2014; Anders et al., 2008). However, there seems to be an association between high BMI and recurrent inguinal hernia (Anuk, 2018). Based on the present study and a review of the literature, it is not clear whether there is an association between PPV and low BMI respective to the development of inguinal hernias. The relationship between recurrent inguinal hernia, high BMI and prior PPV was not examined in this study.
Limitations
Regarding the present work, some investigators may raise concern that clinical examination (i.e., physical examination) and ultrasound study, rather than CT, were used to rule out the presence of asymptomatic inguinal hernia. The availability of CT and nuclear imaging modalities throughout Vietnam is relatively limited. However, studies do confirm that ultrasound can accurately diagnose and rule out occult inguinal hernia in patients (Bradley et al., 2003; Dreuning et al. 2019). Further, it is difficult to measure the intraoperative size of the PPV when performing a laparoscopic surgery. Therefore, in this study the size of PPV was measured in comparison with the tip of suction-irrigation tube of 5 mm. Lastly, some investigators may suggest that the use of pneumoperitoneum could have some influence in increasing the size of PPV. Two studies suggest that pneumoperitoneum may assist in the detection of contralateral PPV (Palmer and Rastinehad, 2007; Onal and Kogan, 2008), but a survey of the literature does not document a study that suggest that pneumoperitoneum will have an effect of increasing the size of a PPV.
CONCLUSION
Asymptomatic PPV has a suggested prevalence of 7.1% in Vietnamese adults, and is more common in males than female and on the right side. PPV can result in a spectrum of pathologies beyond foetal life. Knowledge of the anatomy and embryology (i.e., development and mechanisms of obliteration) of PV and PPV can assist clinicians and ultrasonographers in the evaluation and treatment of patients who present with asymptomatic PPV.
ACKNOWLEDGEMENTS
The authors wish to express their sincere gratitude to the patients who agreed to participate in this investigation. We also wish to thank the surgical technicians of Hue University of Medicine and Pharmacy Hospital (Việt Nam). The authors are appreciative for the editorial assistance and manuscript review of Michael J. Gnezda, B.S., graduate of the Indiana University - Northwest Campus (Gary, IN USA), human cadaver prosector and assistant instructor for human gross anatomy.
Related articles
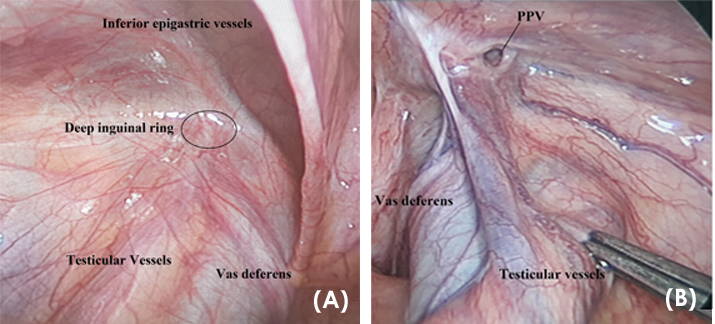 Fig. 1.- Patent Processus Vaginalis (PPV) on the left and the deep inguinal ring in Vietnamese male patients. These views are samples from an unaffected patient and an affected subject in the study cohort. (A) TPLS view of a normal deep inguinal ring (oval). (B) PPV in the area of the deep inguinal ring.
Fig. 1.- Patent Processus Vaginalis (PPV) on the left and the deep inguinal ring in Vietnamese male patients. These views are samples from an unaffected patient and an affected subject in the study cohort. (A) TPLS view of a normal deep inguinal ring (oval). (B) PPV in the area of the deep inguinal ring. 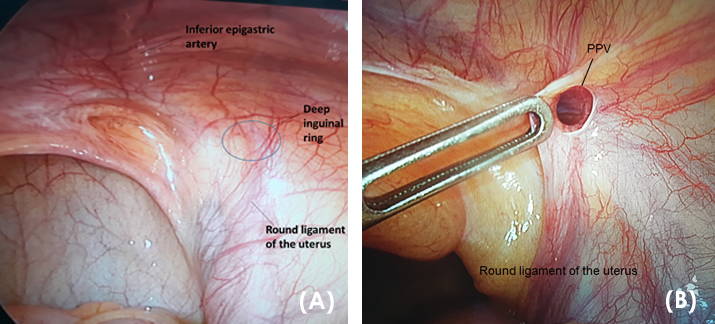 Fig. 2.- Patent Processus Vaginalis (PPV) on the left and the deep inguinal ring in Vietnamese female patients. These sample views are from an unaffected patient, and a sample subject in the study cohort. (A) TPLS view of a normal deep inguinal ring (oval). The region/course of the round ligament of the uterus is observed. (B) PPV in the area of the deep inguinal ring. Passing through the PPV at its proximal location results in entering the Canal of Nuck.
Fig. 2.- Patent Processus Vaginalis (PPV) on the left and the deep inguinal ring in Vietnamese female patients. These sample views are from an unaffected patient, and a sample subject in the study cohort. (A) TPLS view of a normal deep inguinal ring (oval). The region/course of the round ligament of the uterus is observed. (B) PPV in the area of the deep inguinal ring. Passing through the PPV at its proximal location results in entering the Canal of Nuck.Abrahamson J (1998) Etiology and pathophysiology of primary and recurrent groin hernia formation. Surg Clin North Am, 76(6): 953-972.
ANUK T (2018) Factors influencing recurrence in inguinal herniorrhaphy. Ann Med Res, 25(4): 619-622.
Bradley M, Morgan D, Pentlow B, Roe A (2003) The groin hernia - an ultrasound diagnosis?. Ann R Coll Surg Engl, 85(3): 178-180.
BOUZADA J, VAZQUEZ T, DURAN M, DELMAS V, LARKIN T, CUESTA MA, SANUDO J (2017) New insights into the morphogenesis of the gubernaculum testis and the inguinal canal. Clin Anat, 30(5): 599-607.
Brainwood M., Beirne G, Fenech M (2020), Persistence of the processus vaginalis and its related disorders. AJUM, 23(1): 22-29.
Burgu B, Baker LA, Docimo SG (2010) Chapter 43 - cryptorchidism A2 - Gearhart, John P. In: Rink RC, Mouriquand PDE (editors). Pediatric Urology, 2nd ed. W.B. Saunders Philadelphia, pp 563-576.
Cives RV, Casasnovas AB, Martin AA, Arias MP, Sierra RT (1996) The influence of patency of the vaginal process on the efficacy of hormonal treatment of cryptorchidism. Eur J Pediatr, 155(11): 932-936.
Clarnette TD, Hutson J (1999) The development and closure of the processus vaginalis. Hernia, 3: 97-102.
Dreuning KMA, Ten Broeke CEM, Twisk JWR, Robben SGF, Rijn RRV, Verbeke JIML, Van Huren LWE, Derikx JPM (2019) Diagnostic accuracy of preoperative ultrasonography in predicting contralateral inguinal hernia in children: a systematic review and meta-analysis. Eur Radiol, 29(2): 866-876.
Favorito LA, Costa WS, Sampaio FJ (2005) Relationship between the persistence of the processus vaginalis and age in patients with cryptorchidism. Int Braz J Urol, 31(1): 57-61.
Gaeta M, Minutoli F, Mileto A, Racchiusa S, Donato R, Bottari A, Blandino A (2010) Nuck canal endometriosis: MR imaging findings and clinical features. Abdom Imaging, 35(6): 737-741.
George B, Holcomb W, Morgan WM, Brock JW (1996) Laparoscopic evaluation for contralateral patent processus vaginalis: Part II. J Pediatr Surg, 31(8): 1170-1173.
Godbole PP, Stringer MD (2010) Chapter 44 - patent processus vaginalis A2 - Gearhart, John P. In: Rink RC, Mouriquand PDE (editors). Pediatric Urology, 2nd ed. W.B. Saunders Philadelphia, pp 577-584.
Han CH, Kang SH (2002) Epididymal anomalies associated with patent processus vaginalis in hydrocele and cryptorchidism. J Korean Med Sci, 17: 660-662.
Hata S, Takahashi Y, Nakamura T, Suzuki R, Kitada M, Shimano T (2004) Preoperative sonographic evaluation is a useful method of detecting contralateral patent processus vaginalis in pediatric patients with unilateral inguinal hernia. J Pediatr Surg, 39(9): 1396-1399.
Hayes HM, Tarone RE, Cantor KP (1995) On the association between canine malignant lymphoma and opportunity for exposure to 2,4-dichlorophenoxyacetic acid. Environ Res, 70(2): 119-125.
Hayes HM, Tarone RE, Cantor KP, Jessen CR, McCurnin DM, Richardson RC (1991). Case-control study of canine malignant lymphoma: positive association with dog owner’s use of 2,4-dichlorophenoxyacetic acid herbicides. J Natl Cancer Inst, 83(17): 1226-1231.
Hayes HM, Tarone RE, Casey HW, Huxsoll DL (1990) Excess of seminomas observed in Vietnam service U.S. military working dogs. J Natl Cancer Inst, 82(12): 1042-1046.
Holley A (2018) Pathologies of the canal of Nuck. Sonography, 5(1): 29-35.
Hosgor M, Karaca I, Ozer E, Erdag G, Ulukus C, Fescekoglu O, Aikawa M (2004) The role of smooth muscle cell differentiation in the mechanism of obliteration of processus vaginalis. J Pediatr Surg, 39(7): 1018-1023.
Laing FC, Townsend BA, Rodriguez JR (2007) Ovary‐containing hernia in a premature infant: sonographic diagnosis. J Ultrasound Med, 26(7): 985-987.
Lee DGI, Lee YSUK, Park KH, Baek M (2015) Risk factors for contralateral patent processus vaginalis determined by transinguinal laparoscopic examination. Exp Ther Med, 9(2): 421-424.
Mitchell GAG (1939) The condition of the peritoneal vaginal processes at birth. J Anat, 73(Pt 4): 658-661.
Moore KL, Persaud TVN, Torchia MG (2011) Before we are born: Essentials of Embryology and Birth Defects. Elsevier Health Sciences / Mosby, Maryland Heights, Missouri.
Mouravas VK, Koletsa T, Sfougaris DK, Philippopoulos A, Petropoulos AS, Zavitsanakis A, Kostopoulos I (2010) Smooth muscle cell differentiation in the processus vaginalis of children with hernia or hydrocele. Hernia, 14(2): 187-191.
National Academies of Sciences, Engineering, and Medicine (2018) Veterans and Agent Orange: Update 11 (2018). Washington, DC, NAP, https://doi.org/10.17226/25137.
Noguchi D, Matsumoto N, Kamata S, Kaneko K (2014) Ectopic pregnancy developing in a cyst of the canal of Nuck. Obstet Gynecol, 123(2 Pt 2 Suppl 2): 472-476.
Okoshi K, Mizumoto M, Kinoshita K (2017) Endometriosis‐associated hydrocele of the canal of Nuck with immunohistochemical confirmation: a case report. J Med Case Rep, 11(1): 354.
Onal B, Kogan BA (2008) Additional benefit of laparoscopy for nonpalpable testes: finding a contralateral patent processus. Ped Uro, 71(6): 1059-1063.
Palmer LS, Rastinehad A (2008) Incidence and concurrent laparoscopic repair of intra-abdominal testis and contralateral patent processus vaginalis. Urology, 72(2): 297-299.
Rafailidis V, Varelas S, Apostolopoulou F, Rafailidis D (2016) Nonobliteration of the processus vaginalis. Sonography of related abnormalities in children. J Ultrasound Med, 35(4): 805-818.
Rahman N, Lakhoo K (2009) Patent processus vaginalis: a window to the abdomen. Afr J Paediatr Surg, 6(2): 116-117.
Rees MA, Squires JE, Tadros S, Squires JH (2017) Canal of Nuck hernia: a multimodality imaging review. Pediatr Radiol, 47(8): 893-898.
Rosemar A, Angerås U, Rosengren A (2008) Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg, 247(6): 1064-1068.
Rowe MI, Copelson LW, Clatworthy HW (1969) The patent processus vaginalis and the inguinal hernia. J Pediatr Surg, 4(1): 102-107.
Saleem MM (2008) Scrotal abscess as a complication of perforated appendicitis: a case report and review of the literature. Cases J, 1(1): 165:1-4.
Sameshima YT, Yamanari MG, Silva MA, Neto MJ, Funari MB (2017) The challenging sonographic inguinal canal evaluation in neonates and children: an update of differential diagnoses. Pediatr Radiol, 47(4): 461-472.
Shehzad KN, Riaz AA (2011) Unusual cause of a painful right testicle in a 16‐year‐old man: a case report. J Med Case Rep, 5(1): 27:1-3.
Singh AK, Kao S, D’Alessandro M, Sato Y (2010) Case 164: funicular type of spermatic cord hydrocele. Radiology, 257(3): 890-892.
Talarico, Jr. EF, Mas JL, Jones JA (2018) A comprehensive anatomical characterization and radiographic study of stage III testicular cancer in a 31-year-old male patient. Eur J Anat, 22(3): 241-256.
Thandassery RB, Appasani S, Yadav TD, Dutta U, Indrajit A, Singh K, Kochhar R (2014) Implementation of the Asia-Pacific guidelines of obesity classification on the APACHE-O scoring system and its role in the prediction of outcomes of acute pancreatitis: a study from India. Dig Dis Sci, 59(6): 1316-1321.
Van Veen RN, Van Wessem KJP, Halm JA, Simons MP, Plaisier PW, Jeekel J, Lange JF (2007) Patent processus vaginalis in the adult as a risk factor for the occurrence of indirect inguinal hernia. Surg Endosc, 21: 202-205.
Van Wessem KJP, Simons MP, Plaisier MP, Lange JF (2003) The etiology of indirect inguinal hernias; congenital and/or acquired? Hernia, 7(2): 76-79.
Watson RW, Sharp KW, Vasquez JM (1994) Incidence of inguinal hernias diagnosed during laparoscopy. South Med J, 87(1): 23-25.
Weaver KS, Poola AS, Gould JL, Sharp SW, Holcomb GW, St. Peter SD (2016) The risk of developing a symptomatic inguinal hernia in children with an asymptomatic patent processus vaginalis. J Pediatr Surg, 22(1): 60-64.
WHO (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363(9403): 157-163.
Zhao J, Chen Y, Lin J, Jin Y, Yang H, Wang F, Zhong H, Zhu J (2017) Potential value of routine contralateral patent processus vaginalis repair in children with unilateral inguinal hernia. Br J Surg, 104(1): 148-151.