Parahiatal hernias are rare. They are difficult to diagnose preoperatively, as the clinical symptoms may be similar to hiatal and paraoesophageal hernias. Here, we report two cases of parahiatal hernia that were preoperatively diagnosed and successfully repaired laparoscopically; using the particular anatomic characteristics of this hernia, we also review the controversial oesophageal hiatal anatomy, as the surgical community often refers to the left bundle of the right crus as the left crus. There is no consensus on the indication or surgical technique to repair them.
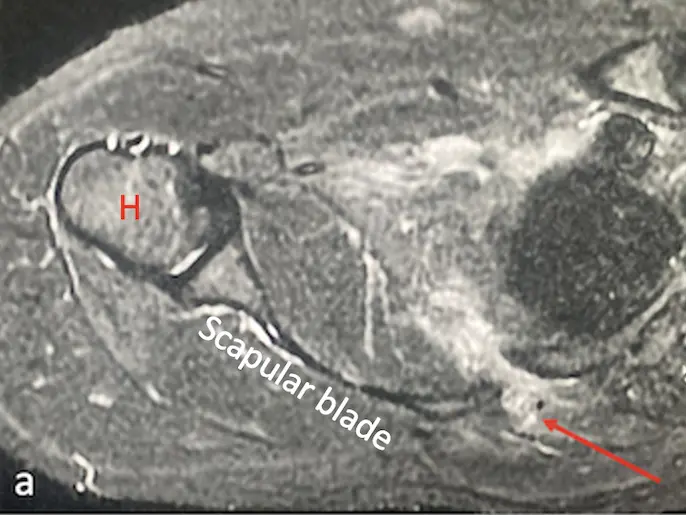
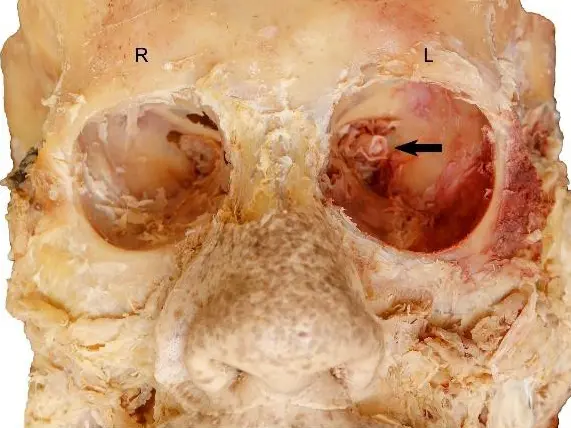
The first case is a 59-year-old woman with non-specific abdominal symptoms, in whom the preoperative gastroscopy and computed tomography (CT) raised the suspicion for parahiatal hernia. The second case is a 68-year-old woman who presented to the emergency department with abdominal distention and nausea, but no vomiting. Preoperative CT raised the suspicion of an incarcerated parahiatal hernia. Both patients underwent laparoscopic repair of the parahiatal hernia and a Toupet fundoplication. They had an uneventful postoperative course. After more than 4 years of follow-up, they are both asymptomatic. Parahiatal hernias are a rare form of diaphragmatic hernia that occur through a diaphragmatic defect lateral to an anatomically normal oesophageal hiatus, with herniation of contents between the left portion of the right crus and the left crus. Up to five different anatomical variations have been described. The knowledge of these anatomical variations has an impact on the type of surgical repair that will need to be performed if a parahiatal hernia is found.