Anatomy knowledge retention is an important consideration in the training of health professionals. In this study, musculoskeletal anatomy knowledge retention was measured in students enrolled in the osteopathic programs at Southern Cross University, Australia. The double-degree osteopathic program has recently undergone curriculum change from five years to four years. Anatomy knowledge in the final-year students of the four-year program was compared to final-year students in the five-year program. Anatomy knowledge amongst the final-year students was also compared to osteopathic practitioners. To measure anatomy knowledge, a test consisting of 20 multiple-choice questions was used, with ten low-order and ten high-order questions, based on the Blooming Anatomy Tool. Students enrolled in the osteopathic program were invited to participate. A total of 92 students participated from a total of 106 students (student response rate of 86.8%). 118 osteopathic practitioners (osteopaths) completed the anatomy knowledge test from a possible 2,546 Australian osteopaths (response rate 4.6%). Retrospective data of anatomy knowledge retention amongst chiropractic students enrolled at Macquarie University, Australia was used to compare with the osteopathic students. There were no differences in the measured level of anatomy knowledge in both low-order and high-order questions between osteopathic students and osteopaths. There were no differences in the measured level of anatomy knowledge in both low-order and high-order questions between senior (fourth-year) students in the four-year program and senior (fifth-year) students in the five-year osteopathic program. The results from this study indicate there is a consistent level of anatomy knowledge retention among osteopathic students and practitioners.
Anatomy knowledge retention in Australian osteopathic training: A comparative study
Raymond Blaich1,2, Nalini Pather3, Tania Prvan4, Roger Engel1, Anneliese Hulme3, Goran Strkalj3
1 Department of Chiropractic, Faculty of Medicine, Health and Human Sciences’, Macquarie University, Sydney, Australia
2 School of Health and Human Sciences, Southern Cross University, Lismore, New South Wales, Australia
3 Department of Anatomy, School of Medical Sciences, Faculty of Medicine, University of New South Wales, Sydney, Australia
4 Department of Mathematics and Statistics, Faculty of Science and Engineering, Macquarie University, Sydney, Australia
SUMMARY
Sign up or Login
Abbreviations
Anatomy knowledge retention (AKR)
Australian Osteopathic Accreditation Council (AOAC)
Bachelor of Clinical Sciences (BClinSc)
Basic Competency Examination (BCE)
Master of Osteopathic Medicine (MOM)
Musculoskeletal (MSK)
Progress Test in Medicine (PTM)
Southern Cross University (SCU)
Macquarie University (MU)
Low-Order (LO)
High-Order (HO)
INTRODUCTION
Anatomy has long been considered an essential foundation in the training of medical and health practitioners (Turney, 2007, Louw et al., 2009; Ahmed et al., 2010; Diaz-Mancha et al., 2016; Estai & Bunt, 2016; Dayal et al., 2017; Losco et al., 2017; Farey et al.,2018; Blaich et al., 2019). The study of anatomy aids in preparing students for clinical practice (Sugard et al., 2010; Valenza, 2012) not only through teaching about the structures of the human body, but also in the development of non-traditional discipline-independent skills (Rizzolo, 2010; Lachman and Pawlina, 2006; Strkalj, 2014; Evans et al., 2018; Hildebrandt, 2019). These skills include professionalism, time-management, empathy, teamwork, and respect for the patient (Swartz, 2006; Bockers et al., 2010; Talarico, 2010; White et al., 2011; Talarico, 2012).
In health profession programs, anatomy education is predominantly delivered in the first two years of training. In these early years, biomedical sciences dominate the curricula, giving way to more clinically oriented disciplines later in the program (Strkalj, et al., 2011; Nabil et al., 2014; McBride and Drake, 2018; Giuriato, et al., 2019; Arantes et al., 2020; Lufler et al., 2020). This type of delivery leads to a time interval between the initial acquisition of biomedical knowledge such as anatomy and the clinical application of that knowledge (Lufler et al., 2020). Anatomy knowledge retention (AKR) is therefore an important factor to consider when designing programs for health professional education.
AKR is a complex domain. Numerous studies have demonstrated anatomy knowledge attrition (i.e., a decrease in anatomy knowledge) in the latter stages of health profession programs (Feigin et al., 2002; Prince et al., 2005; Feigin et al., 2007; Lazarus et al., 2012; Jurjus et al., 2014; Brunk et al., 2017; Farey et al., 2018; Lufler et al., 2020). However, others have shown an increase in AKR as students’ progress through their programs (Humphreys et al., 2007; Hulme et al., 2019).
With recent significant changes in the content and delivery of anatomy within medical and health professions education (McBride and Drake, 2016; Day et al., 2018; Lufler et al., 2020), concerns have been raised about the level of AKR of students as they graduate and move into clinical practice (McKeown et al., 2003; Prince et al., 2005; Humphreys et al., 2007; Ahmed et al., 2010; Bergmann et al., 2011; Strkalj et al., 2011; Jurjus et al., 2014; Meyer et al., 2015; Doomernik et al., 2017). These concerns extend to a broad range of health professions, including chiropractic (Stkalj et al., 2011), podiatry (Diaz-Mancha et al., 2016), optometry (Backhouse et al., 2019), and nursing (Narnaware and Neumeier, 2020).
In addition, other factors that can influence AKR such as vertical integration of anatomy knowledge within curricula (Bergman et al., 2011; Parmar and Rathinam, 2011; Bergman et al., 2014), composition of assessments (Blunt and Blizzard, 1975; Feigin et al., 2002; Feigin et al., 2007; Jurjus et al., 2016), anatomy curricula requiring specific clinical context (D’Eon et al., 2006; Kerfoot et al., 2007; Custers, 2010; Dobson and Linderholm, 2015; Karpicke and Blunt, 2011; Karpicke, 2012; Smith et al., 2016; Dobson et al., 2017; Dayal et al., 2017; Williams and Mann, 2017; Castillo et al., 2018; Farey et al., 2018) and their cumulative effect on AKR have not been fully explored.
Assessing the effect of these factors is important for designing strategies to improve AKR. Different assessment tools have been used to assess AKR. These include the Progress Test in Medicine (PTM) (Brunk et al., 2017), the Basic Competency Examination (BCE) (Freedman and Bernstein, 1998; Childs, et al., 2005; Stockard and Allen, 2006), the carpal and tarsal bone tests (Valenza et al., 2012; Diaz-Mancha et al., 2016), and Bloom’s taxonomy-ordered multiple-choice questions (Hulme et al., 2019). While these studies produced valuable results in AKR assessment of different student cohorts, the use of different assessment tools hampered the comparison of AKR across disciplines and pedagogies. However, using the same AKR assessment tool on students from different discipline programs, and different educational institutions, demonstrated differences in levels of anatomy knowledge at similar stages of progression (Wass et al., 2001; Humphreys et al., 2007; Valenza et al., 2012; Brunk et al., 2016; Daiz-Mancha et al., 2016). This suggests that anatomy education within the health professions is a complex issue and that AKR may be dependent on both the anatomical region studied and the perceived importance of that anatomical region to the specific health discipline.
Studies focusing on AKR in medical (McKeown et al., 2003; Valenza et al., 2012; Nabil et al., 2014), physical therapy (Diaz-Muncha et al., 2016; Parmar and Rathinam, 2011; Valenza et al., 2012), podiatry (Castillo-Lopez et al., 2014), nursing (Zieber and Sedgewick, 2918; Narnaware and Neumeier, 2020), occupational therapy (Parmar and Rathinam, 2011), chiropractic (Strkalj et al., 2011), and osteopathic students (Stockard and Allen, 2006) did not compare levels of AKR with clinicians. Other studies focused on AKR in just clinicians such as medical practitioners (Spielmann and Oliver, 2005; Custers and Cute, 2011; Roche et al., 2011; Farey et al., 2018) and optometrists (Bakkum and Trachimowicz, 2015). These latter studies demonstrated that attrition of anatomy knowledge increased with time since graduation (Spielmann and Oliver, 2005; Custers and Cute, 2011; Bakkum and Trachimowicz, 2015). However, to date there has been only one investigation into AKR of musculoskeletal (MSK) anatomy in osteopathic students (Stockard and Allen, 2006), and no study of AKR in osteopathic practitioners within an Australian context.
This study had two aims. The first aim was to provide a preliminary assessment of musculoskeletal anatomy knowledge in the final-year osteopathic students at an Australian tertiary university, and thus their preparedness (in terms of anatomy knowledge) to enter the workforce. This was achieved through the comparison of the results of anatomy tests (focusing on the anatomy of limbs at two different cognitive levels) completed by the final-year osteopathic students and a sample of practicing osteopaths. In addition, test results of the final year students were compared with those of the final year chiropractic students from Macquarie University (MU). This comparison was considered valid because of the similarities between the two health professions, both focusing on musculoskeletal disorders and relying on manual therapy. The second aim was to assess anatomy knowledge of the final year students in two osteopathic programs, the old five-year program and the new four-year program.
MATERIALS AND METHODS
Student data was collected from students enrolled in the Master of Osteopathic Medicine (MOM) degree at Southern Cross University (SCU) in Lismore, New South Wales, Australia. Data were collected from osteopathic practitioners via an online discussion forum. The osteopathic program at SCU is a double-degree program consisting of an undergraduate Bachelor of Clinical Sciences (BClinSc) and a postgraduate MOM. Students must successfully complete both degrees to register as an osteopath in Australia. Both degrees are accredited with the Australian Osteopathic Accreditation Council (AOAC, 2020), the body responsible for osteopathic education accreditation in Australia.
The osteopathic program at SCU has recently undergone curriculum change through which duration to complete the double-degree program decreased from five to four years effectively reducing the MOM from two years to one year. The new, revised BClinSc degree remained three years in duration. The first student intake into the new four-year program commenced in February 2017. The main curriculum change in the new integrated program is that education is delivered and assessed within a clinically-oriented context with greater emphasis on evidence-based practice. The change included streamlining delivery to remove repetitious content, thereby improving the overall integration of the curriculum. This included the anatomical curriculum.
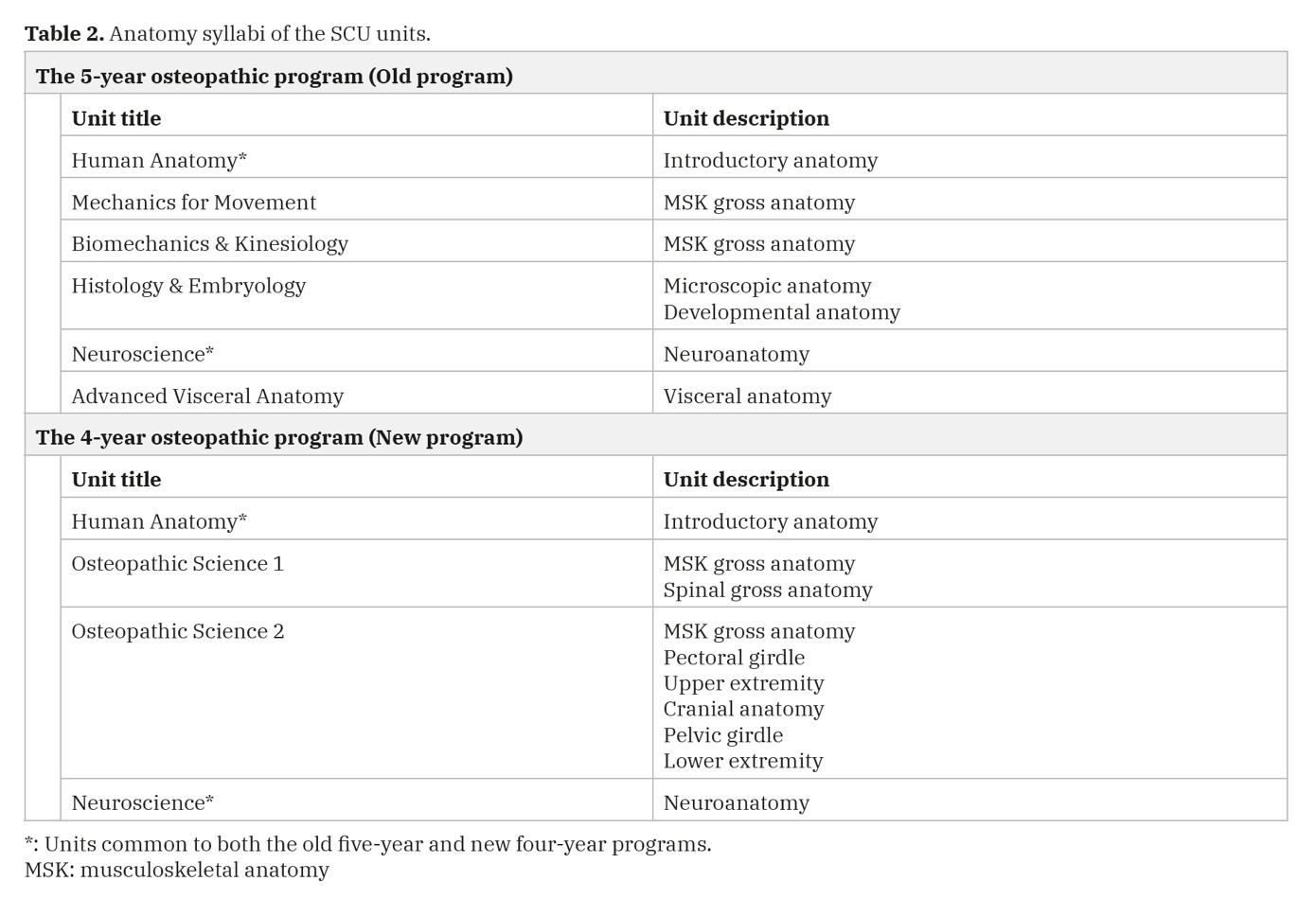
Anatomy curriculum at Southern Cross University
The anatomy curriculum in the revised program includes several anatomy units (subjects or courses) spread over two teaching sessions per year. The university has three 13-week teaching sessions per academic year). All units follow a common format and include face-to-face lectures (1 hour per week), tutorials (1 hour per week) and anatomy laboratory practical classes with prosected specimens (2 hours per week). The exception to this is the histology and embryology unit which does not have practical classes. Table 1 outlines the anatomy units in the old five-year and new four-year osteopathic programs at SCU.
Table 2 describes the content of each of the units listed in Table 1. In session 1 of year one in the new four-year program, there is a shared introductory unit covering the basic concepts of anatomy. Two osteopathic specific units (Osteopathic Science 1 and Osteopathic Science 2) are delivered in session 2 of year 1 and session 1 of year 2. These units include an in-depth study of the functional, clinical and biomechanical anatomy of each anatomical region. Osteopathic Science 1 covers the vertebral column (axial skeleton), and visceral anatomy while Osteopathic Science 2 covers the pectoral girdle and upper limb, pelvic girdle, lower limb, and the cranium. Student learning is supported by online resources delivered via the Blackboard learning management system (Blackboard Inc. Version 3.9.2). Students can access these online resources at any time and are used for both summative and formative assessment activities.
Participant Population
Participants in this study were the senior osteopathic students (both fifth-year students in the old five-year program and fourth-year students in the new four-year program) in the osteopathic programs at SCU and osteopathic practitioners working in private practice. Student data was collected from students enrolled in the MOM at SCU in Lismore, Australia. Eligible students were invited to participate during scheduled classes. Introducing the new four-year course while the old five-year course was being ‘taught out’ meant that there were two cohorts of students studying the same material at different stages of their respective courses. Table 3 details the different student cohorts and the stage of their respective programs.
Data were collected from osteopathic practitioners via two avenues: an online discussion forum, and direct paper-based. Collected data included age, gender, and year of graduation. Online osteopathic practitioners were recruited Australia-wide via an online forum. This online forum was sponsored by Osteopathy Australia, the osteopathic profession’s peak professional body. For the direct approach, ten osteopathic practitioners attending a local osteopathic educational meeting, were invited to participate.
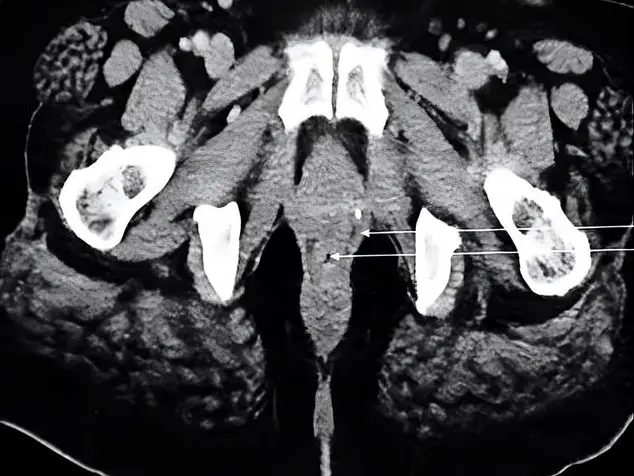
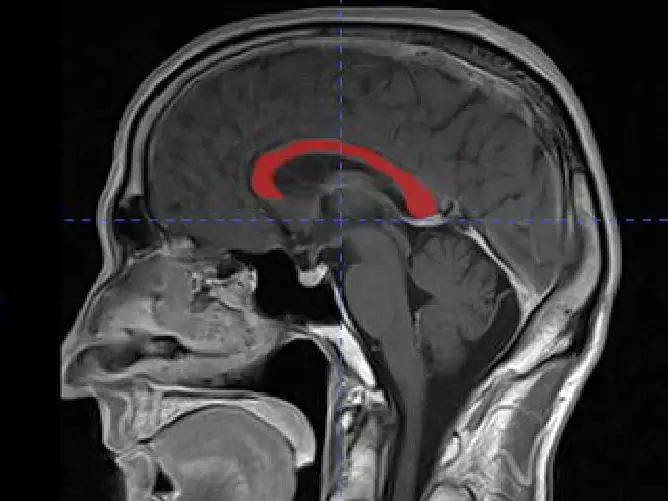
The Test Instrument
To measure anatomy knowledge, a 20-question test instrument in a multiple-choice format was used that assessed knowledge of musculoskeletal (MSK) anatomy of the upper and lower limbs. This instrument had originally been developed and validated to assess the MSK anatomical knowledge of chiropractic students at Macquarie University in Sydney, Australia (Hulme et al., 2019). The test consisted of two components: 10 lower cognitive order (Low-order LO) questions requiring simple recall of anatomical detail; and 10 higher cognitive order (High-order HO) questions requiring analysis, application and integration of anatomy knowledge as it pertained to a clinical setting. The LO and the HO questions were evenly distributed throughout the test to improve compliance by avoiding participants’ becoming discouraged when encountering more difficult questions (HO) mid-test. The classification into two cognitive orders was based on the Blooming Anatomy Tool, a set of discipline specific criteria utilising Bloom’s Taxonomy that classifies cognitive levels of anatomy knowledge for multiple-choice questions (Anderson et al., 2001; Thompson and O’Loughlin, 2015; Morton et al., 2017; Day, 2018). Students were given the opportunity to participate in class with no prior warning to prevent biasing the results through pre-test preparation. Participating students were asked to keep the test questions confidential from other students. All data were de-identified.
Participant recruitment and Data collection
Student data were collected near the end of the 2020 academic year (November). Fourth- and fifth year-students were invited to participate during one of their final classes for the year. They were informed that the test was not a summative assessment and did not count towards their final grade in the unit. Students were provided with a written copy of the test and given 20 minutes to complete it.
Osteopathic practitioners asked to participate in this study were recruited by both direct and indirect means. Direct means involved contact with the chief investigator at a local osteopathic educational gathering in 2019. Practitioners were invited to participate and provided with a hard copy of the test if they agreed to participate and provide consent. The indirect approach involved inviting practitioners to participate via an online discussion forum run by the national osteopathic association in 2020. Participation was voluntary and anonymous. There was no personal identification information collected from any of the participants as part of this study.
Statistical Analysis
Data were recorded and collated using MS Excel (Microsoft Corporation, version 16, 2016). All statistical calculations were performed using Statistical Package for Social Sciences (SPSS), version 23 (IBM Corp, Armonk, NY). Descriptive data, including means and standard deviations were calculated where appropriate. Mean scores were calculated for the correct number of low-order, high-order and total questions answered. Data were compared using paired t-tests. A p-value of less than 0.005 was considered statistically significant (i.e., using 0.5 % significance) for all analysis.
Ethics Approval
Ethics approval to collect data for this study was provided by two Human Research Ethics Committees (HRECs): Southern Cross University (approval number: ECN-14-242) and Macquarie University (Reference number: 52020907722092).
RESULTS
Participants
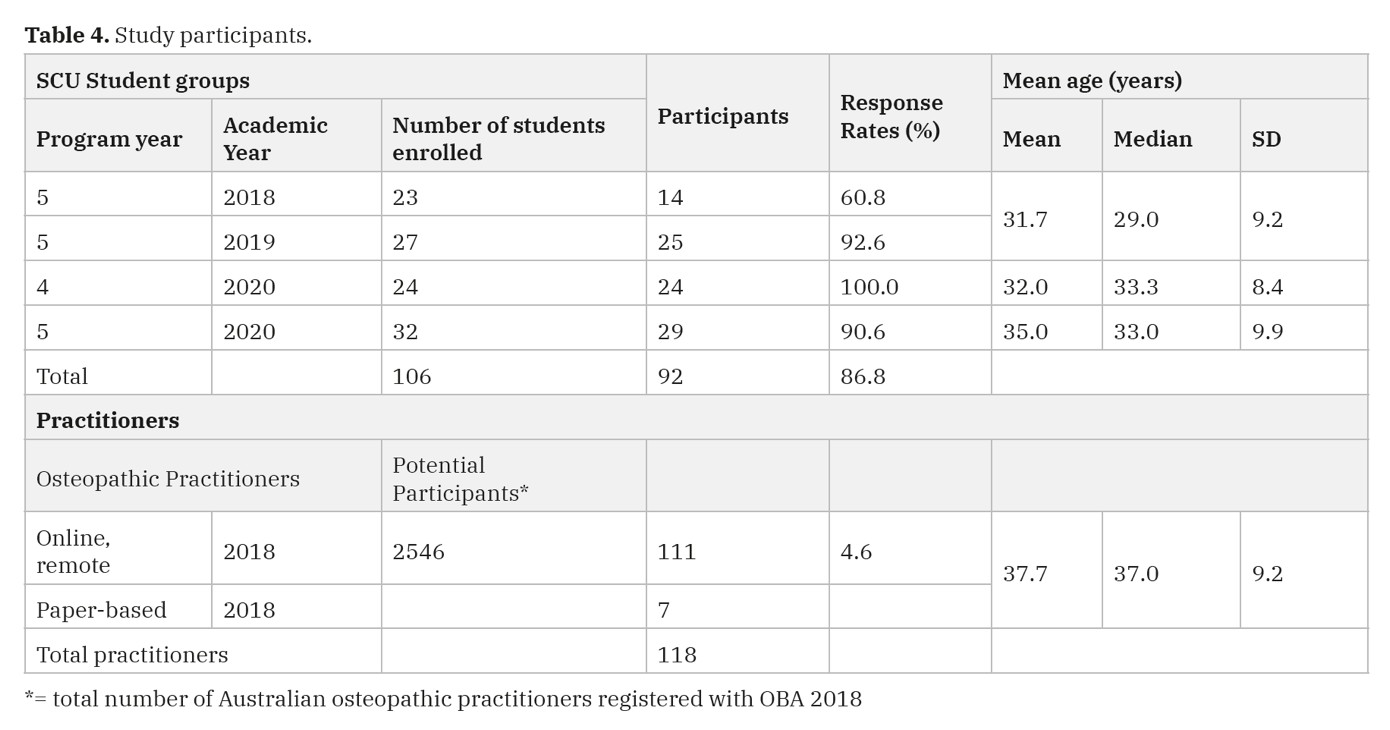
In total, 224 participants completed the questionnaires (106 students and 118 practitioners). For the students, this represented an 86.8% response rate (Table 4). According to the Australian Health Practitioner Regulation Agency (AHPRA), there were 2,546 registered osteopathic practitioners in Australia as of 30th of June 2018 (OBA, 2020). A total of 118 practitioners completed the questionnaire: 111 online and 7 paper-based, representing a response rate of 4.6% (118/2546).
Comparison of knowledge retention of students and practitioners
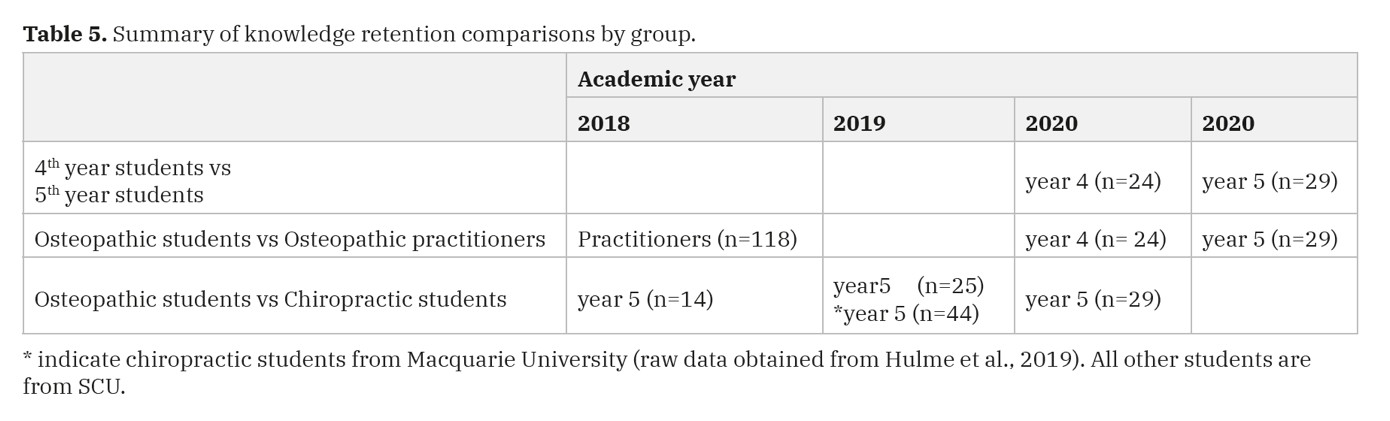
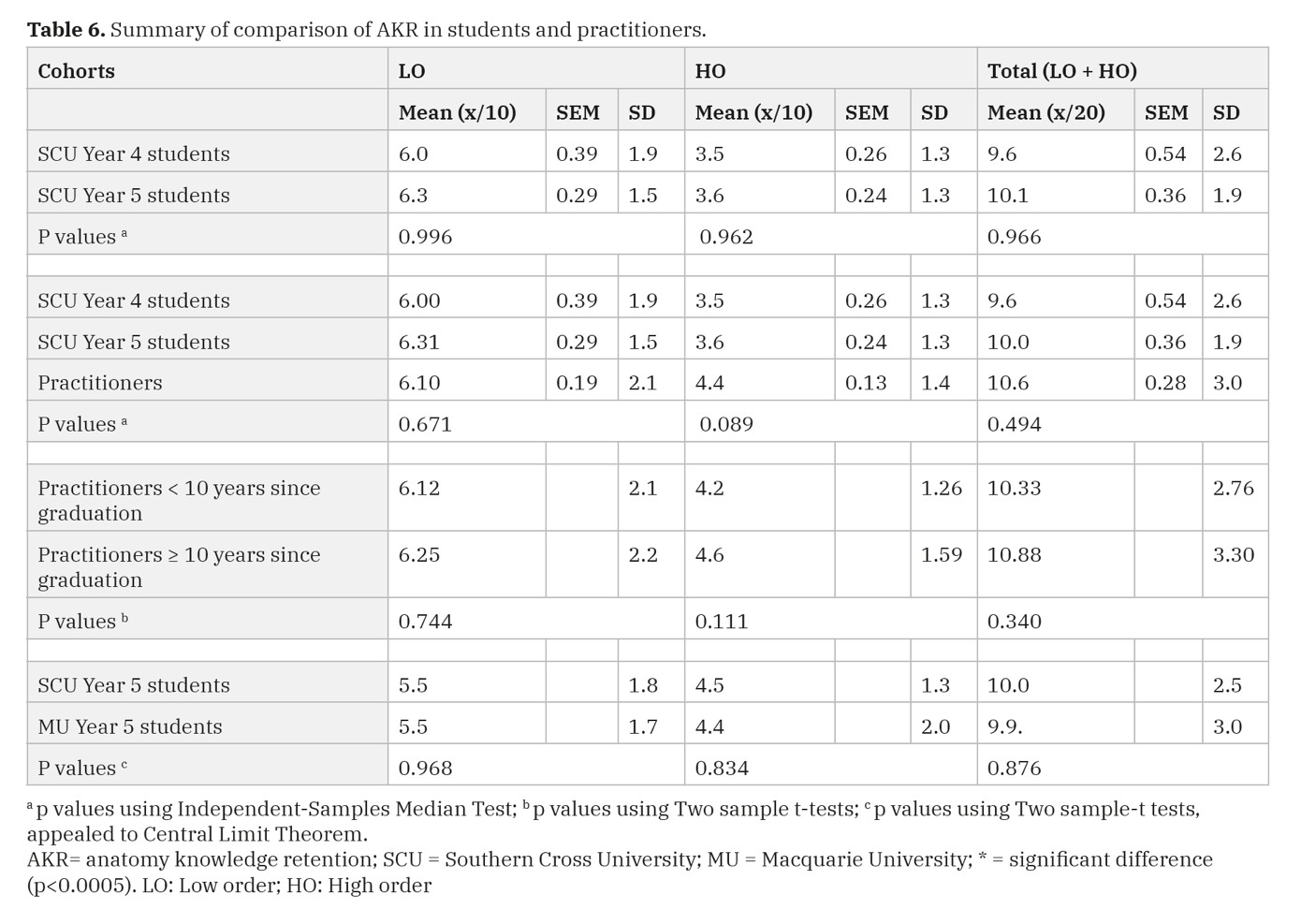
To ascertain whether there were differences between anatomy knowledge of osteopathic students, osteopathic practitioners, and chiropractic students at a different institution, knowledge retention was assessed using LO and HO questions. Using the independent-samples median test, scores were compared for the following (Tables 5 and 6):
Final-year osteopathic students in 2020: Year-four and Year-five.
Final-year osteopathic students in 2020 and osteopathic practitioners.
Year-5 final-year osteopathic students at SCU to Year-5 final-year chiropractic students at Macquarie University (MU).
Retrospective comparisons were also made with previous data of AKR among chiropractic students (Hulme et al., 2019) and compared with SCU students.
There were no differences between the fifth-year osteopathic students and fifth-year chiropractic students. All other comparisons revealed no differences in scores (LO, HO or total: LO + HO).
Age & Gender differences
There were no gender differences in any of the participant populations. There was a difference in the mean age of practitioners compared to both student groups (year 2 and year 5). While this is not surprising given, a practitioner in Australia would have to be of post-graduate age.
DISCUSSION
A major objective of educating health practitioners is the development of a sound knowledge -base which can be readily applied, integrated and synthesised to a clinical setting. The measurement of AKR can be used as a way of assessing whether this educational objective has been achieved. This study evaluated AKR in osteopathic students and osteopathic practitioners. The results demonstrated little attrition of knowledge amongst students and practitioners. Comparison between osteopathic and chiropractic students at a similar stage in their programs showed there was a difference in AKR.
Anatomy knowledge and program length
There were no differences in student mean scores, between the shorter four-year program and the longer five -year program at SCU implying students appeared to be equally effective in learning anatomy over a shorter duration. These results are not surprising as the new SCU anatomy curriculum was designed to be vertically integrated. This is consistent with the findings from similar studies (McBride and Drake, 2016; Wilson et al., 2018; Hulme et al., 2019; Zhao et al., 2020) that measured anatomy knowledge in medical students enrolled in an integrated problem-based learning curriculum (McBride and Drake, 2016; Wilson et al., 2018; Zhao et al., 2020), and chiropractic students enrolled in a standard program (Hulme et al., 2019).
The results from the present study provide evidence that graduates of a four-year osteopathic program are as ready to enter the health care workforce as those from a five-year program, with respect to their knowledge of MSK anatomy. This conclusion supports the change to a shorter program at SCU.
The results can be explained by the configuration of the new four-year program with its integrated curriculum where biomedical and clinical sciences are taught within a more clinically oriented context (Brauer et al., 2015; Johnston and Vaughan, 2020). Although there is still a pre-dominance of biomedical sciences in the early years of the program followed by clinical learning in the later years (Craig et al., 2010; Talarico and Painter, 2020), the integrated approach includes clinical context for the content covered in the earlier years so as to enhance learner engagement and content retention (Erkonen et al., 1992; Norman, 2009; Bridges et al., 2016; Quintero et al., 2016; Farey et al., 2018).
AKR in osteopaths
It was expected that there would be difference in AKR between students and practitioners and that anatomy knowledge attrition would increase with length in time in practice (Bakkum and Trachomowicz, 2015). Surprisingly, there were no differences in AKR between osteopaths and senior students and no attrition of anatomy knowledge in osteopaths. The findings of the present study contradict findings from other studies that investigated AKR in health practitioners (Custers and Cate, 2011; Bakkum and Trachimowicz (2015). These studies demonstrated decreasing AKR over time. Bakkum and Trachimowicz (2015) studied knowledge of the microanatomy of the retina in fourth-year optometry students (n=35), optometry faculty members (n=41) and optometrists in private practice (n=96), and found a steady and consistent trend of knowledge attrition with years from graduation. The longer the private practice optometrists had been in practice, the less retinal layers they were able to correctly identify.
In a study of AKR in medical students (n= 25) and practicing doctors (n=25; junior doctors: n=15; senior doctors: n=10), the doctors were able to correctly identify more of the carpal bones compared to the medical students (Spielmann and Oliver, 2006). Furthermore, the senior doctors with more clinical experience performed better than the medical students and junior doctors. This is to be expected, although caution is advised, as this study used a very small sample size and the carpal bones test is a crude and very limited measure of anatomy knowledge. A study also using the carpal bones test found similar results (i.e., poor AKR) in medical graduates (n=102) undertaking specialty-training in Accident & Emergency medicine, or trauma/orthopaedics (Roche et al., 2011).
The discrepancy in results from these studies and the present study can be explained by the different anatomy knowledge measurement tool used. The present study used the MSK anatomy knowledge test, which is a more comprehensive measurement of anatomy knowledge compared to the narrow carpal bone test, which is limited in its ability to measure anatomy knowledge.
Using a knowledge test covering a range of basic biomedical sciences including anatomy, physiology, biochemistry, and pathophysiology, a long-term study of medical students (n=65) and medical practitioners (n=75) reported better performances by students compared to practitioners with length in practice a contributing factor (Custers and Cate, 2011). Similarly, licensed physical therapists (n=182) scored better than physical therapy students on the BCE tool (Childs et al., 2005), supporting the concept that there is a difference between anatomical knowledge and clinical competency with that knowledge (Jassen et al., 2014). In an Australian study that also used the BCE to measure MSK knowledge in general practitioners (n=47) and orthopaedic interns (n=66), general practitioners scored higher (Broadhurst et al., 2002). These results are to be expected as the BCE assesses clinical management as well as MSK anatomy knowledge and general practitioners had experienced broader clinical management than the orthopaedic interns. Taken together the choice of test may be a factor in determining results in an AKR test and could explain the difference in results in the present study. The context of the curriculum and the emphasis placed on the learners’ perception of the relevance of the anatomy being taught may also affect the level of AKR (Bergman et al., 2014).
Comparison between osteopathic and chiropractic students
As there are many similarities between the scope of practice of chiropractic and osteopathy, it was considered appropriate to compare AKR among students from the two professions. Both professions focus on the MSK system and related disorders and share a common reliance on manual therapy as an intervention. Data on AKR in chiropractic students at MU has been reported in the literature and was made available to the researchers (Hulme et al., 2019). Data from fifth-year chiropractic students at MU was compared to performances with fifth-year osteopathic students at SCU.
There were no differences in AKR between the fifth-year osteopathic and chiropractic students. It was anticipated that both fifth-year student cohorts would perform similarly in the AKR test, as these students were at the conclusion of their formal studies and about to enter the workforce as health practitioners.
Both programs included integrated curricula (Hulme et al., 2019) and both had received full accreditation by the relevant accrediting bodies. The difference in AKR in students could be attributed to the anatomy syllabus component of the new osteopathic (four-year) program.
Our findings are consistent with similar comparisons of AKR in students in other health professions. These include studies using the carpal bone test in fifth-year Australian chiropractic students (n=44), who did much better than second-year chiropractic students (n=47) (Meyer et al., 2015); fifth-year chiropractic students (n=84) who did much better than final-year medical students (Strkalj et al., 2011); and third-year Spanish physical therapy (PT) students (n= 54) who did better than third-year Spanish medical students (n=80) (Valenza et al. (2012). Contradicting these results, Dayal et al. (2017) found that first-year Australian physiotherapy students (n=129) were better at correctly identifying the carpal bones compared to their fourth-year (n=113) counterparts. In a study of Spanish podiatry students (first-years n=145 and fourth-years n=109), Castillo-Lopez et al. (2014) found no difference in anatomy knowledge when using the tarsal bones test. These conflicting findings can be explained by the use of different tests, both of which are a narrow measure of AKR that is not indicative of other components of anatomy knowledge.
Limitations
It is important to state that AKR as measured in the present study does not equate to clinical competency. Even though HO questions were included, these questions do not give any indication of clinical competency. Measuring clinical competency is more complex than measuring AKR (Miller 1990; Wass et al., 2001). The format and nature of anatomy assessment can strongly influence anatomy learning and AKR (Logan et al., 2011; Bergman et al., 2014). This study did not include how anatomy was assessed within the programs, or the timing of anatomy assessments.
This study only measured AKR and did not investigate the factors which could influence AKR. Further studies should include focus groups with osteopathic students to discuss factors in anatomy learning that they consider important to improve AKR and better prepare them for clinical practice (Bergman et al., 2014; Farey et al., 2018). These factors could then be used by curricula planners to improve anatomy learning outcomes.
All data gathered as part of this study was cross-sectional in nature. Longitudinal data of AKR would provide more methodological rigour and validity. Measuring AKR in the same student cohorts at multiple time points would help to achieve this.
This study was not designed to be a comprehensive assessment of all AKR at a single educational institution (e.g., SCU). The test instrument used in this study was limited to only measuring MSK anatomy knowledge. Other aspects of the anatomy curriculum were not measured such as the sub-disciplines visceral anatomy, spinal anatomy, microanatomy (histology), developmental anatomy (embryology), neuroanatomy, and radiographic anatomy. Measuring what constitutes a passable or satisfactory mean test score, or what level of anatomy knowledge could be considered as ample for safe and effective osteopathic clinical practice were considered beyond the scope of this study and therefore not identified.
As participation in this study was voluntary and did not from part of the formal anatomy assessments, the number of participants in the various student cohorts may not be representative of the entire student cohort. As all data used in this study was obtained anonymously, it was not possible to measure an individual’s performance over time with only mean scores used for comparisons. The small student sample sizes are a result of the small number of students enrolled in the osteopathic programs at SCU and could be considered a limitation with respect to the generalisability of these results.
The study also used a small number of MCQs as the knowledge retention assessment tool.
The theory-based MCQs are easy and quick to mark, eliminate potential bias, and increase inter-examiner reliability. This tool may not thoroughly assess anatomy knowledge and it is recommended that a more comprehensive set of questions be used in future studies in order to assess anatomy knowledge more thoroughly.
Future Directions
As these results may not be comparable with other educational institutions, further investigations could include conducting similar studies at other osteopathic educational institutions in Australia and overseas to validate these findings on a broader scale. Additionally, expanding the scope of assessments to include other parts of the anatomy curriculum, e.g., visceral anatomy, spinal anatomy, histology, embryology, and neuroanatomy, would improve our understanding of anatomy knowledge retention. To improve anatomy knowledge amongst students, others have suggested the addition of anatomy instructions where students revisit key anatomical concepts so as to improve their ability to transfer anatomy knowledge to a clinical setting (Lazarus et al., 2012; Jurjus et al., 2016).
CONCLUSION
There is a consistent level of anatomy knowledge retention among Australian osteopathic students and practitioners. Shortening the length of an osteopathic program does not appear to affect the level of musculoskeletal anatomy knowledge in graduating students in a vertically integrated curriculum. The results from the present study can assist in informing the development of a core anatomy curriculum for osteopathic education within the Australian context, and can also contribute to the standardisation of a minimum level of anatomy knowledge required for students entering clinical practice.
Related articles
AHMED K, ROWLAND S, PATEL V, KHAN RS, ASHRAFIAN H, DAVIES DC, DARZI A, ATHANASIOU T, PARASKEVA PA (2010) Is the structure of anatomy curriculum adequate for safe medical practice? Surgeon, 8(6): 318-324.
ANDERSON LW, KRATHWOHL DR, AIRASIAN PW, CRUIKSHANK KA, MAYER RE, PINTRICH PR, RATHS J, WITTROCJ MC (2001) A taxonomy for learning, teaching, and assessing: A revision of Bloom’s taxonomy of educational objectives. Abridged 1st Ed. Allyn & Bacon, Boston, MA, pp 352.
ARANTES M, ANDRADE JP, BARBOSA J, FERREIRA MA (2020) Curricular changes: The impact on medical students’ knowledge of neuroanatomy. BMC Med Educ, 20(1): 20.
AUSTRALIAN OSTEOPATHIC ACCREDITATION COUNCIL (2020) Accreditation. 2016 http://www.osteopathiccouncil.org.au/accreditation.html, [Accessed: 18/12/20]
BACKHOUSE S, TAYLOR D, ARMITAGE JA (2019) Is this mine to keep? Three-dimensional printing enables active, personalized learning in anatomy. Anat Sci Educ, 12(5): 518-528.
BAKKUM BW, TRACHOMOWICZ RA (2015) Retention of knowledge of retinal microanatomy by optometric students, faculty, and practitioners. Optometric Educ, 40(2): 77-82.
BERGMAN EM, VAN DER VLEUTEN CP, SCHERPBIER AJ (2011) Why don’t they know enough about anatomy? A narrative review. Med Teach, 33(5): 403-409.
BERGMAN EM, DE BRUIN AB, HERRLER A, VERHEIJEN IW, SCHERPBIER AJ, VAN DER VLEUTEN CP (2013) Student’s perceptions of anatomy across the undergraduate problem-based learning medical curriculum: A phenomenographical study. BMC Med Educ, 13(1): 151-152.
BERGMAN EM, VERHEIJEN IW, SCHERPBIER AJ, VAN DER VLEUTEN CP, DE BRUIN AB (2014) Influences on anatomical knowledge: The complete arguments. Clin Anat, 27(3): 296-303.
BERGMAN EM, DE BRUIN AB, VORSTENBOSCH MA, KOOLOOS JG, PUTS GC, LEPPINK J, SCHERPBIER AJ, VAN DER VLEUTEN CP (2015) Effects of learning content in context on knowledge acquisition and recall: A pretest-posttest control group design. BMC Med Educ, 15(1): 133.
BLAICH R, PATHER N, LUO K, STRKALJ G (2019) Australian osteopathic practitioners’ perceptions of the clinical relevance of anatomy. Inter J Morph, 37(1): 319-323.
BLUNT MJ, BLIZARD PJ (1975) Recall and retrieval of anatomical knowledge. Med Educ, 9(4): 255-263.
BOCKERS A, JERG-BRETZKE L, LAMB C, BRINKMANN A, TRAUE HC, BOCKERS TM (2010) The gross anatomy course: An analysis of its importance. Anat Sci Educ, 3(1): 3-11.
BRAUER DG, FERGUSON KJ (2015) The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach, 37(4): 312-322.
BRIDGES S, YIU CKY, BOTELHO MG (2016) Design considerations for an integrated, problem-based curriculum. Med Sci Educ, 26(3): 365-373.
BRUNK I, SCHAUBER S, GEORG W (2017) Do they know too little? An inter-institutional study on the anatomical knowledge of upper-year medical students based on multiple choice questions of a progress test. Ann Anat, 209: 93-100.
CASTILLO-LOPEZ JM, DIAZ-MANCHA JA, HEREDIA-RIZO AM, FERNANDEZ-SEGUIN LM, POLO-PADILLO J, DOMINGUEZ-MALDONADO G, MUNUERA PV (2014) The tarsal bone test: A basic test of health sciences students’ knowledge of lower limb anatomy. BioMed Res Int, 2014: 939163.
CASTILLO JM, PARK YS, HARRIS I, CHEUNG JJH, SOOD L, CLARK MD, KULASEGARAM K, BRYDGES R, NORMAN G, WOODS N (2018) A critical narrative review of transfer of basic science knowledge in health professions education. Med Educ, 52(6): 592-604.
CHILDS JD, WHITMAN JM, SIZER PS, PUGIA ML, FLYNN TW, DELITTO A (2005) A description of physical therapists’ knowledge in managing musculoskeletal conditions. BMC Musculoskel Disorders, 6(1): 32.
CRAIG S, TAIT N, BOERS D, McANDREW D (2010) Review of anatomy education in Australia and New Zealand medical schools. ANZ J Surg, 80(4): 212-216.
CUSTERS EJ (2010) Long-term retention of basic science knowledge: a review study. Adv Health Sci Educ, 15(1): 109-128.
CUSTERS EJ, CATE OTJ (2011) Very long-term retention of basic science knowledge in doctors after graduation. Med Educ, 45: 422-430.
DAY LJ (2018) A gross anatomy flipped classroom effects performance, retention, and higher-level thinking in lower performing students. Anat Sci Educ, 11(6): 565-574.
DAYAL MR, OWENS O, GIBSON W, STRKALJ G (2017) Anatomical knowledge retention in physiotherapy students: A preliminary assessment. Int J Anat Res, 5(1.2): 3474-3479.
D’EON MF (2006) Knowledge loss of medical students on first year basic science courses at the University of Saskatchewan. BMC Med Educ, 6(1): 5.
DIAZ-MANCHA JA, CASTILLO-OPEZ JM, MUNUERA-MARTINEZ PV, FERNANDEZ-SEGUIN LM, POLO-PADILLO J, HEREDIA-RIZO AM (2016) A comparison of fourth-year health science student’s knowledge of gross lower and upper limb anatomy: A cross-sectional study. J Manip Physiol Ther, 39(6): 450-457.
DOBSON JL, LINDERHOLM T (2015) The effect of selected “desirable difficulties” on the ability to recall anatomy information. Anat Sci Educ, 8(5): 395-403.
DOBSON JL, PEREZ J, LINDERHOLM T (2017) Distributed retrieval practice promotes superior recall of anatomy information. Anat Sci Educ, 10(4): 339-347.
DOOMERNIK DE, VAN GOOR H, KOOLOOS JG, TEN BROEK RP (2017) Longitudinal retention of anatomical knowledge in second-year medical students. Anat Sci Educ, 10(3): 242-248.
DRAKE RL (2007) A unique, innovative, and clinically oriented approach to anatomy education. Acad Med, 82(5): 475-478.
ERKONEN WE, ALBANESE MA, SMITH WL, PANTAZIS NJ (1992) Effectiveness of teaching radiologic image interpretation in gross anatomy: A long-term follow-up. Invest Radiol, 27(3): 264-266.
ESTAI M, BUNT S (2016) Best teaching practices in anatomy education: A critical review. Ann Anat, 208: 151-157.
EVANS DJ, PAWLINA W, LACHMAN N (2018) Human skills for human[istic] anatomy: An emphasis on nontraditional discipline -independent skills. Anat Sci Educ, 11(3): 221-224.
FAREY JE, BUI DT, TOWNSEND D, SURESHKUMAR P, CAR S, ROBERTS C (2018) Predictors of confidence in anatomy for work as a junior doctor: A national survey of Australian medical students. BMC Med Educ, 18(1): 174.
FEIGIN D, MAGID D, SMIRNIOPOULOS J, CARBOGNIN S (2007) Learning and retaining normal radiographic chest anatomy does preclinical exposure improves student performance? Acad Radiol, 14(9): 1137-1142.
FEIGIN DS, SMIRNIOTOPULOS JG, NEHER TJ (2002) Retention of radiographic anatomy of the chest by 4th-year medical students. Acad Radiol, 9(1): 82-88.
FREEDMAN KB, BERNSTEIN J (1998) The adequancy of medical school education in musculoskeletal medicine. J Bone Joint Surgery, 80-A(10): 1421-1427.
GIURIATO R, STRKALJ G, MEYER AJ, PATHER N (2019) Anatomical sciences in chiropractic education: A survey of chiropractic programs in Australia. Anat Sci Educ, 13(1): 37-47.
HILDEBRANDT S (2019) The role of history and ethics of anatomy in medical education. Anat Sci Educ, 12(4): 425-431.
HULME AK, LUO K, STRKALJ G (2019) Musculoskeletal anatomy knowledge retention in the Macquarie University chiropractic program: A cross-sectional study. Anat Sci Educ, 13(2): 182-191.
HUMPHREYS BK, SULKOWSKI A, McINTYRE K, KASIBAN M, PATRICK AN (2007) An examination of musculoskeletal cognitive competency in chiropractic interns. J Manip Physiol Ther, 30(1): 44-49.
JANSSEN SA, VAN DER MEULEM SP, SHOSTROM VK, LOMNETH CS (2014) Enhancement of anatomical learning and developing clinical competence of first-year medical and allied health profession students. Anat Sci Educ, 7(3): 181-190.
JOHNSON S, VAUGHAN B (2020) ‘We need one more hour solely based on anatomy…. Give us anatomy!’: Early-year learner perceptions of anatomy within an integrated and case-based learning osteopathy curriculum. Intern J Osteo Med, 36: 49-54.
JURJUS RA, LEE J, AHLE S, BROWN KM, BUTERA G, GOLDMANN EF, KRAPF JM (2014) Anatomical knowledge retention in third-year medical students prior to obstetrics and gynecology and surgery rotations. Anat Sci Educ, 7(1): 461-468.
JURJUS RA, BROWN RA, GOLDMAN E, GALOOSIAN A, BUTERA G, KRAPF JM (2016) Curricular responses to increase recall and transfer of anatomical knowledge into the obstetrics/gynecology clerkship. Anat Sci Educ, 9(4): 337-343.
KARPICKE JD (2012) Retrieval-based learning: Active retrieval promotes meaningful learning. Curr Dir Psychol Sci, 21(3): 157-163.
KARPICKE JD, BLUNT JR (2011) Retrieval practice produces more learning than elaborative studying with concept mapping. Science, 331(6018): 772-775.
KERFOOT BP, DE WOLF WC, MASSER BA, CHURCH PA, FEDERMAN DD (2007) Spaced education improves the retention of clinical knowledge by medical students: A randomised controlled trial. Med Educ, 41(1): 23-31.
LACHMAN N, PAWLINA W (2006) Integrating professionalism in early medical education: The theory and application of reflective practice in the anatomy curriculum. Clin Anat, 19(5): 456-460.
LAZARUS MD, CHINCHILLI VM, LEONG SL, KAUFFMAN GLJ (2012) Perceptions of anatomy: Critical components in the clinical setting. Anat Sci Educ, 5(4): 187-199.
LOGAN JM, THOMPSON AJ, MARSHAK DW (2011) Testing to enhance retention in human anatomy. Anat Sci Educ, 4(5): 243-248.
LOSCO CD, GRANT WD, ARMSON A, MEYER AJ, WALKER BF (2017) Effective methods of teaching and learning anatomy as a basic science: A BEME systematic review: BEME Guide no. 44. Med Teach, 39(3): 234-243.
LOUW G, EIZENBERG N, CARMICHAEL SW (2009) The place of anatomy in medical education: AMEE Guide no 41. Med Teach, 31(5): 373-386.
LUFLER RS, LAZARUS MD, STEFANIK JJ (2020) The spectrum of learning and teaching: The impact of a fourth-year anatomy course on medical student knowledge and confidence. Anat Sci Educ, 13(1): 19-29.
McBRIDE JM, DRAKE RL (2016) Longitudinal cohort study on medical student retention of anatomical knowledge in an integrated problem-based learning curriculum. Med Teach, 38(12): 1209-1213.
McBRIDE JM, DRAKE RL (2018) National survey on anatomical sciences in medical education. Anat Sci Educ, 11(1): 7-14.
McKEOWN PP, HEYLINGS DJA, STEVENSON M, McKELVEY KJ, NIXON JR, McCLUSKEY D (2003) The impact of curricular change on medical students’ knowledge of anatomy. Med Educ, 37(11): 954-961.
MEYER AJ, ARMSON A, LOSCO CD, LOSCO B, WALKER BF (2015) Factors influencing student performance on the carpal bone test as a preliminary evaluation of anatomical knowledge retention. Anat Sci Educ, 8(2): 133-139.
MILLER GE (1990) The assessment of clinical skills/competence/performance. Acad Med, 65(9 Suppl): S63-S67.
MORTON DA, COLBERT-GETZ JM (2016) Measuring the impact of the flipped anatomy classroom: The importance of categorizing an assessment by Bloom’s taxonomy. Anat Sci Educ, 10(2): 170-175.
NABIL NM, AL-MOUSLY N, OUSLY, N. AlWATHNANI S, ABDULDAIEM A, AL-ISSA H (2014) Medical Students’ perception on anatomy knowledge relevance and retention during clerkship. J Contemp Med Educ, 2(3): 147-151.
NARNAWARE Y, NEUMEIER M (2020) Second-year nursing students’ retention of gross anatomical knowledge. Anat Sci Educ, 13(2): 230-236.
NORMAN G (2009) Teaching basic science to optimize transfer. Med Teach, 31(9): 807-811.
OSTEOPATHY BOARD OF AUSTRALIA (2020) 2019/2020 Annual Report. Retreived from https://www.osteopathyboard.gov.au/News/Annual-report.aspx [Assessed 21/11/20]
PARMAR SK, RATHINNAM BA (2011) Introduction of vertical integration and case-based learning in anatomy for undergraduate physical therapy and occupational therapy students. Anat Sci Educ, 4(3): 170-173.
PRINCE KJ, SCHERPBIER AJ, VAN MAMEREN H, DRUKKER J, VAN DER VLEUTEN CP (2005) Do students have sufficient knowledge of clinical anatomy? Med Educ, 39(5): 326-332.
QUINTERO GA, VERGEL J, ARREDONDO M, ARIZA M-C, GOMEZ P, PINZON-BARRIOS A-M (2016) Integrated medical curriculum: Advantages and disadvantages. J Med Educ Curricular Devel, 2016(3): 133-137.
RAUPACH T, ANDERSEN JC, MEYER K, STROBEL L, KOZIOLEK M, JUNG W, BROWN J, ANDERS S (2016) Test-enhanced learning of clinical reasoning: A crossover randomised trial. Med Educ, 50(7): 711-720.
RIZZOLO L, RANDO W, O’BRIEN M, HAIMS A, ABRAHAMS J, STEWART W (2010) Design, implementation, and evaluation of an innovative anatomy course. Anat Sci Educ, 3(3): 109-120.
ROCHE A WILLIAMS G, WHARTON D, BROWN D (2011) Physical and radiographic identification of the bones of the wrist by junior doctors. J Hand Surg Eur, 36(2): 107-110.
SMITH MA, BLUNT JR, WHIFFEN JW, KARPICKE JD (2016) Does providing prompts during retrieval practice improve learning? Appl Cognit Psychol, 30(4): 544-553.
SPIELMANN PM, OLIVER CW (2005) The carpal bones: A basic test of medical students’ and junior doctor’s knowlegde of anatomy. Surgeon, 3(4): 257-259.
STOCKARD AR, ALLEN TW (2006) Competence levels in musculoskeletal medicine: Comparison of osteopathic and allopathic medical graduates. J Am Osteop Assoc, 106(6): 350-355.
STRKALJ G (2014) The emergence of humanistic anatomy. Med Teach, 36(10): 912-913.
STRKALJ G, SCHRODER T, PATHER N, SOLYALI V (2011) A Preliminary assessment of the fifth-year chiropractic students’ knowledge of anatomy. J Altern Complement Med, 17(1): 63-66.
SUGARD K, ABRAHAMS P, KHURANA A (2010) The anatomy of anatomy: A review for its modernization. Anat Sci Educ, 3(2): 83-93.
SWARTZ WJ (2006) Using gross anatomy to teach and assess professionalism in the first year of medical school. Clin Anat, 19(5): 437-441.
TALARICO Jr EF (2010) A human dissection training program at Indiana university school of medicine-northwest. Anat Sci Educ, 3(2): 77-82.
TALARICO Jr EF (2012) A change in paradigm: Giving back identity to donors in the anatomy wet laboratory. Clin Anat, 26(2): 161-172.
TALARICO Jr EF, PAINTER SD (2020) Small team-based medical imaging of human cadavers: An innovative tool for interdisciplinary learning in human gross anatomy and radiologic scineces. Eur J Anat, 24(2): 141-154.
THOMPSON AR, O’LOUGHLIN VD (2015) The blooming taxonomy tool (BAT): A discipline-specific rubric for utilising Bloom’s taxonomy in the design and evaluation of assessments in the anatomical sciences. Anat Sci Educ, 8(6): 493-501.
TURNEY BW (2007) Anatomy in a modern medical curriculum. Ann R Coll Surg Engl, 89(2): 104-107.
VALENZA MC, CASTRO-MARTIN E, VALENZA G, GUIRAO-PINEIRO M, DE-LA-LLAVE-RINCON AI, FERNANDEZ-DE-LAS-PENAS C (2012) Comparison of third-year medical and physical therapy students’ knowledge of anatomy using the carpal bone test. J Manip Physiol Therap, 35(2): 121-126.
WASS V, VAN DER VLEUTEN C, SHATZER J, JONES R (2001) Assessment of clinical competence. Lancet, 357(9260): 945-949.
WHITE MT, BORGES NJ, GEIGER S (2011) Preceptions of factors contributing to professional identity development and speciality choice: A survey of third and fourth-year medical students. Ann Behav Sci Med Educ, 17(1): 18-23.
WILLIAMS AD, MANN BD (2017) Improved knowledge gain and retention for third-year medical students during surgical journal club using basic science review. A pilot study. Am J Surg, 213(2): 238-243.
WILSON JS, ALVAREZ J, DAVIES BC, DUERINCKX AJ (2018) Cost-effective teaching of radiology with pre-clinical anatomy. Anat Sci Educ, 11(2): 96-206.
ZHAO X, GOLDMAN E, BANANI T, KLINE K, BROWN K, LEE J, JUJUS RA (2020) The process of curricular integration and its effects on anatomical knowledge retention. Clin Anat, 33(6): 960-968.
ZIEBER M, SEDGEWICK M (2018) Competence, confidence and knowledge retention in undergraduate nursing students. A mixed method study. Nurse Educ Today, 62: 16-21.