Most of the studies published on the palmaris longus (PL) prevalence are by physical examination methods. None of the reported prevalence studies in Arab populations are based on ultrasonography; hence we have undertaken this study. Our study was performed on 79 (34 male and 45 female) young/adult Arabs. The occurrence of PL tendon was recorded by a physical examination method (Schaeffer’s test), followed by ultrasound measurement of the thickness, width and circumference of the PL tendon at the wrist and the distance between the PL tendon and the median nerve at the wrist, bilaterally. Of 158 wrists examined, the physical examination method revealed the presence of PL tendon in 138 (87.3%) subjects, whereas the ultrasound method revealed 149 (94.3%). Schaeffer’s test gave a false-negative result for 11 cases. The thickness, width and circumference of the PL tendon at the wrist were: 1.14±0.44 mm (right side) & 1.19±0.41 mm (left side); 4.08±1.34 mm (right side) & 4.36±1.26 mm (left side); 8.98±2.94 mm (right side) & 9.45±2.67 mm (left side), respectively. Gender differences in the thickness, width and circumference of the PL tendon at the wrist were: 1.31±0.42 mm (male) and 1.06±0.40 mm (female); 4.61±1.23 mm (male) and 3.93±1.29 mm (female); 10.04±2.59 mm (male) and 8.60±2.82 mm (female), respectively. The distance of the PL tendon from the median nerve (measured 2 cm proximal to distal wrist crease) were: 1.30±0.63 mm & 1.24±0.61 mm on right & left sides; 1.40±0.60 mm & 1.17±0.62 mm in male and females, respectively. The ultrasonographic measurements were statistically significant among genders, while no such significance was detected between the sides. This study has documented both topographic and ultrasonographic description of the PL tendon in a Gulf Arab population; ultrasonography is more reliable for detecting the PL tendon than Schaeffer’s test.
Physical and ultrasonographic examination of palmaris longus tendon in the Arabian Gulf Region
Bhagath K. Potu1, Ahmad A. Alnaggar2, 3, Ayesha Fatima1, Abdel H. Salem1, Raouf A. Fadel1
1 Department of Anatomy, College of Medicine & Medical Sciences, Arabian Gulf University, Kingdom of Bahrain
2Consultant in Radiology, Zagazig University, Egypt & 3Royal Bahrain Hospital, Kingdom of Bahrain
SUMMARY
Sign up or Login
INTRODUCTION
The palmaris longus (PL) is a slender, elongated muscle located medial to the flexor carpi radialis (FCR). It originates from the medial epicondyle, the epicondylar ridge of the humerus, from the adjacent intermuscular septa and the antebrachial fascia. It terminates as a long-slender flattened tendon, which passes over the flexor retinaculum and inserts on the central part of the flexor retinaculum and palmar aponeurosis. The morphology of PL is extremely variable (Clemente, 1985). Reports have shown that the PL may be absent, duplicated, triplicated, reversed or presented as a digastric muscle with various insertions. It has been observed from various studies that the PL is inserted into the fascia of the forearm, the hypothenar eminence, the tendon of the flexor carpi ulnaris muscle, the abductor pollicis brevis, into the carpal tunnel or Guyon’s canal, the pisiform bone and the scaphoid bone (Lalit et al., 2014). The presence of the PL can be assessed by various physical examination methods (Schaeffer, 1909) such as Schaeffer’s test, Pushpakumar’s test, Thomson’s test, Mishra’s test, Reimann test, Gangata test, Hiz test, Bhattacharya test, Lotus sign and four finger sign test. These have been used to confirm the presence of PL in various populations (Pushpakumar et al., 2004; Thompson et al., 1921; Mishra, 2001; Reimann et al., 1994; Gangata, 2009; Hiz et al., 2011). Since there are many other bulky muscles in the forearm to flex the wrist, its absence does not seem to have any functional loss on the biomechanical functions of the wrist region. Moreover, PL is dispensable, so it is the best choice for grafts in tendon reconstruction (Ozasa et al., 2018), lip augmentation (Trussler et al., 2008) and penile reconstruction surgeries (Garaffa et al., 2013). The extent of absence of PL reported in humans varies in different populations. Its absence was reported for the first time by Columbus in De Re Anatomica, cited by Schaeffer (Schaeffer, 1909). PL has been studied extensively using various examination methods, and prevalence of its agenesis varies significantly across the different population from 0.6% to 64% (0.6% in Koreans, 1.02% in Ugandans, 2.9% in Asians, 3-4.3% in Japanese, 3.3-17.2% in Brazilian, 4.5-22.5% in African Americans, 4.5-50.8% in Egyptians, 2.1-4.6% in Chinese, 4.4-32.2% in Hungarians, 5.8-15.2% in Canadians, 6.7-25% in Nigerians, 9.3-11.7% in Malaysians, 11.6% in Czechs, 13.2-33.7% in Iranians, 18.3% in Iraqis, 20.2-37% in Indians, 24% in North American Caucasians, 25% in Irish, 16.7-40.5% in Saudi and Bahraini population of Arabian Gulf region, and highest reported is 15-64% in Turkish population) as mentioned in a meta-analysis (Pekala et al., 2017). A recent meta-analysis based on 19 cadaveric studies revealed that the overall absence of the PL is about 10.3%. With regards to gender, females have been reported to have higher absence, 14.5%, as compared to 6.0% in males. 49 studies in which the function of PL was assessed, the overall absence of PL was 15.6%: males had a pooled absence of PL in 15.1% and17.6% in females (Pekala et al., 2017).
It is important to note that the PL tendon lies immediately superficial to the median nerve at the level of the wrist. When a variant PL is present, its proximity to the median nerve places the latter at risk during tendon harvesting procedures. The median nerve is also more vulnerable to misidentification in patients with congenital absence of the PL tendon. Therefore, safe harvesting of the PL requires a thorough understanding of the relevant anatomy, particularly the relevant anatomical distances, as well as distinguishing the nerve from tendon. There are reports of surgical errors while harvesting the median nerve instead of the PL tendon (Choo et al., 2017; Vastamaki, 1987; Weber and Mackinnon, 2007; Leslie et al., 2017), suggesting that the accurate preoperative assessment of the tendon-nerve relationship is crucial to minimize the risk of such devastating complications. A recent report revealed that the preoperative clinical examination to document the presence of PL did not prevent the accidental erroneous excisions of the median nerve during PL harvest. Hence, more effective methods of estimating graft dimensions must be explored in patients requiring PL tendon grafting (Leslie et al., 2017). A reliable preoperative assessment is only possible through the imaging techniques. The efficacy and reliability of ultrasound measurements to predict PL graft dimensions, however, has not been evaluated comprehensively.
Although few studies (Sater et al., 2010; Raouf et al., 2013; Alzahrani et al., 2017; Alkhamis et al., 2017) were done in the past using physical examination methods on Arab populations, none of these have studied the prevalence and morphological features of PL using the ultrasonography. The objectives of our study were to: (1) determine the presence of PL in Gulf Arabs with physical and ultrasound examination, and (2) perform the morphometry of the PL tendon (thickness, width, and circumference) at the wrist and measure its distance from the median nerve using ultrasonography technique.
MATERIALS AND METHODS
Sample
This study was carried out from February 2019 to March 2020 at Anatomy-Pathology Learning Resource Center (APLRC), Arabian Gulf University, Kingdom of Bahrain. The study subjects were medical students (n= 79, Male: 34; Female: 45) of age between 19-24 years, from the Gulf Co-operative Council (GCC) countries. The number of subjects from different Gulf Arab nations is listed in Table 1. The sample excluded the subjects who had a history of hand surgery or abnormality of the upper limbs. This study was approved by Institutional Research & Ethics Committee (Project number G-E011-PI-11/18). The participation in the study was voluntary, and written informed consent was obtained from all the subjects before performing the procedures.
Physical examination
For examining the PL tendon, a standard testing method “Schaeffer’s test” was used. Subjects were asked to place their thumb against their little finger while flexing the wrist (Fig. 1A). With this test, presence or absence of the PL tendon on both right and left sides were registered.
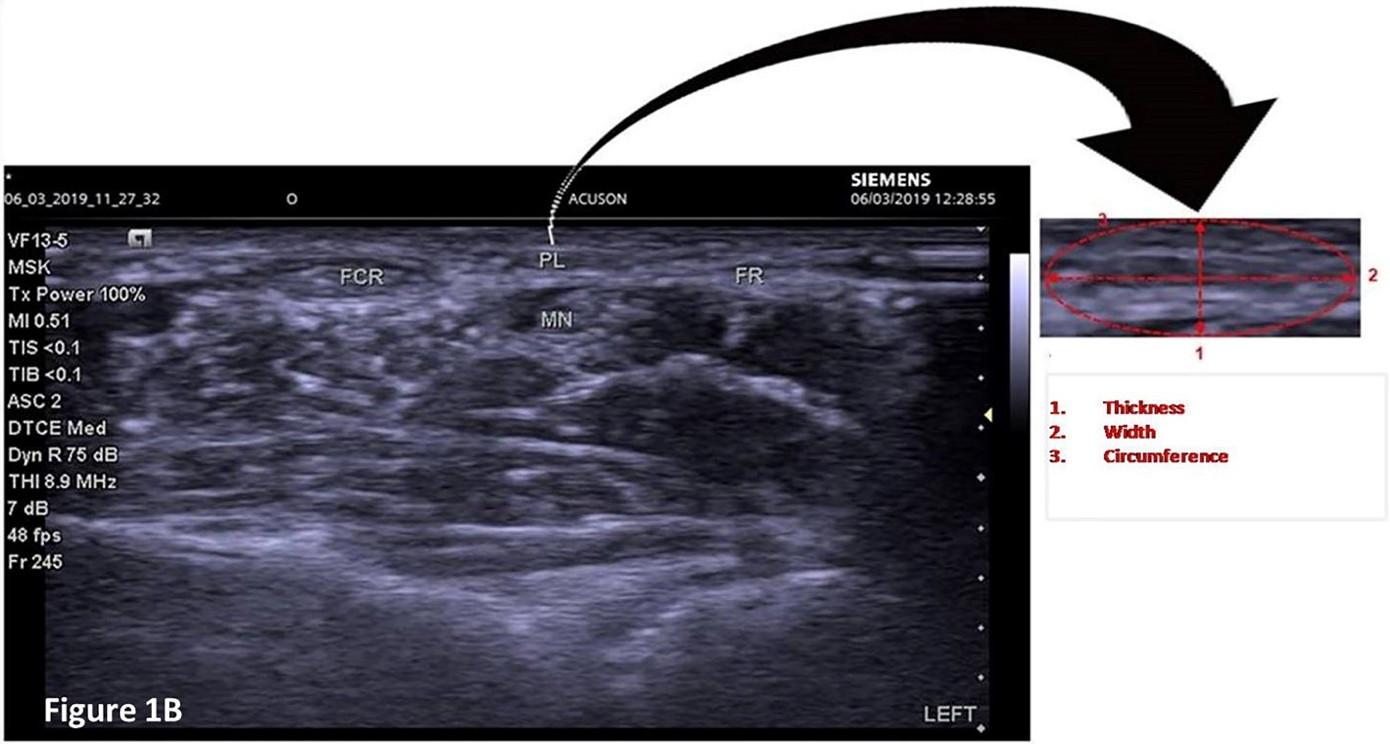
Ultrasound evaluation
Irrespective of the PL tendon finding on physical examination, all subjects underwent ultrasonographic evaluation on “SIEMENS ACUSON P 500 Ultrasound System” located in anatomy lab, College of Medicine & Medical Sciences, Arabian Gulf University. Ultrasonography was performed to indicate the presence of PL tendon and to measure its thickness, width and circumference at the wrist. In addition to the above parameters, the distance of the PL tendon from the median nerve at the wrist (2 cm proximal to distal wrist crease) was also measured. This protocol was adopted from Ertem et al. (2010) (Fig. 1B). Ultrasonography was performed by an experienced radiologist with an array probe with the frequency of 6-15 MHz, which is appropriate for the superficial structures.
Statistical analysis
All statistical analyses were performed using SPSS version 23 (SPSS Inc., USA). Measurements are presented as mean and SD. Chi-square test was performed to see whether any significant differences between the outcomes of physical examination and ultrasonography findings. To examine the gender differences in means of the parameters studied, we have used two sample independent t-test.
RESULTS
Prevalence (Physical and Ultrasound examination)
In our study of 158 wrists, 138 wrists revealed the presence of the PL tendon by physical examination method (87.3%) whereas absent in 20 wrists (12.7%).
Of 34 male subjects (68 wrists) (Table 1), the Schaeffer’s test demonstrated that the PL tendon was present in 60 wrists (88.2%): 42.6% in 29 right wrists and 45.5% in 31 left wrists. Of 8 absent cases (11.7%): 5 were on the right side (7.35%) and 3 were on the left side (4.41%). Whereas in 45 female subjects (90 wrists) (Table 1), Schaeffer’s test demonstrated that the PL tendon was present in 78 wrists (86.6%): 41.1% in 37 right wrists and 45.5% in 41 left wrists. Of 12 absent cases (13.3%): 8 were on the right side (8.88%) and 4 were on the left side (4.44%) (Table 1).
The ultrasound examination also involved the same subjects of the Schaeffer’s test. 149 of 158 wrists demonstrated the presence of the PL tendon by ultrasound examination method (94.3%) while absence was registered in 9 wrists (5.7%).
Of 34 male subjects (68 wrists) (Table 1), the ultrasound evaluation demonstrated that the PL tendon was present in 66 wrists (97%): 47.05% in 32 right wrists and 50% in 34 left wrists. About the 2 absent cases (2.9%): both were on the right side while reporting zero percent cases on the left side. Whereas in 45 female subjects (90 wrists) the ultrasound evaluation demonstrated that the PL tendon was present in 83 wrists (92.2%): 45.5% in 41 right wrists and 46.6% in 42 left wrists (Table 1). Of the seven wrists in which absence was registered (7.7%): 4 were on the right side (4.4%) and 3 were on the left side (3.3%). Overall, the Schaeffer’s test gave a false-negative result for 11 subjects. No anatomical variations in the structure of the PL tendon, such as duplicated tendon or reversed PL muscle, were detected. Chi-square test results showed that the differences between the outcomes of physical examination and ultrasonography were significant (p= 0.032).
PL tendon morphometry by ultrasonographic evaluation
The thickness, width and circumference of the PL tendon and its distance from the median nerve measured at the wrist of all limbs by ultrasound are expressed as Mean±SD. For all the parameters measured, the Bahraini, Omani, Kuwaiti and Saudi samples did not show any statistically significant differences (p>0.05) among right and left sides, except the width and circumference, which were statistically significant in the Bahraini sample (p=0.036; p=0.04) (Table 2). The gender differences in morphometric measurements performed on the PL tendon by ultrasonography are expressed as Mean±SD in Table 3. The overall mean differences of morphometric measurements performed on PL tendon by ultrasonography in both genders are statistically significant for thickness (p<0.0005); width (p=0.001); circumference (p=0.001) and distance between the PL tendon and the median nerve (p=0.023) (Table 3). Data showed that the thickness, width, circumference of the PL tendon and its distance from median nerve were greater on the left side, except the distance of the PT from median nerve in females (Table 4).
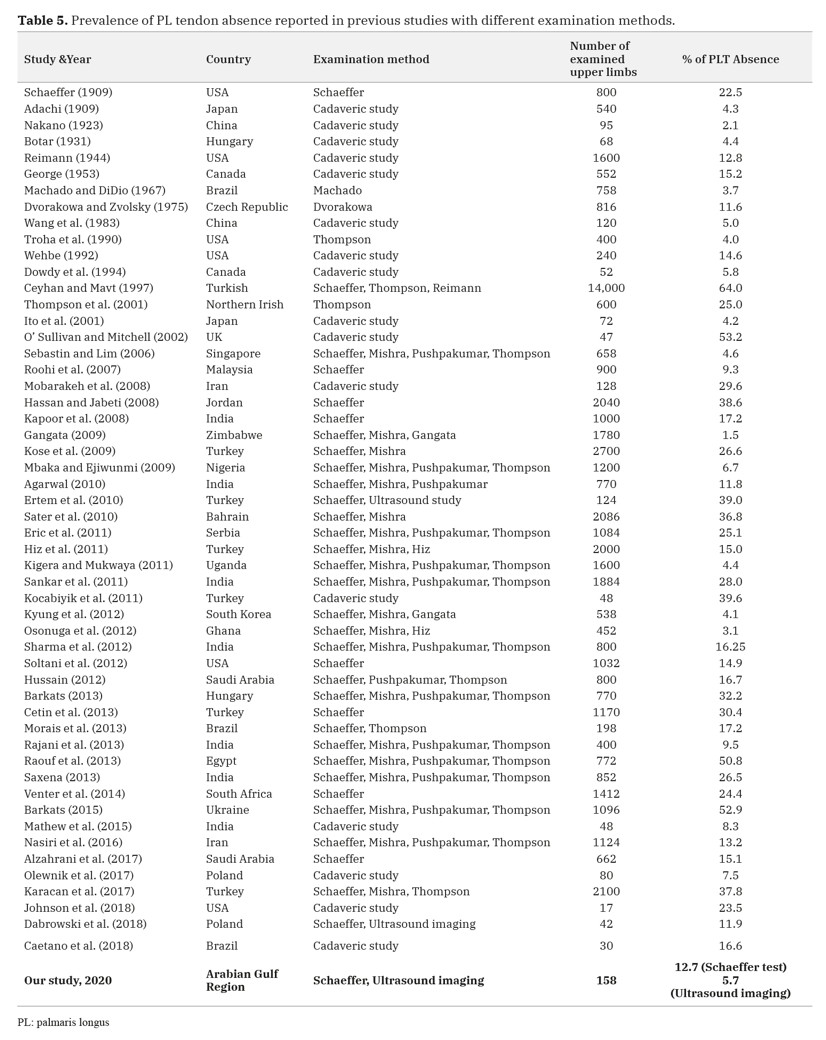
DISCUSSION
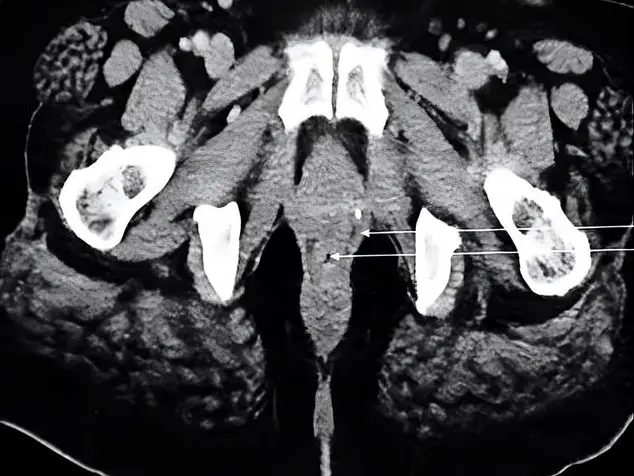
Our study documented absence of the PL tendon in 12.7% of the wrists by physical examination and 5.7% of wrists by ultrasonography. Few previous studies conducted on Arab populations, on the basis of physical examination, showed extreme variation in its occurrence: PL was absent in 38.6% of studied Jordanians (Hassan and Jabeti, 2008); 50.8% in Egyptians (Raouf et al., 2013); 40.5% in Saudis (Alkhamis et al., 2017); 36.8% in Bahrainis (Sater et al., 2010). A subsequent study in Saudi Arabia, however, concluded a much lower rate (16.7%) of PL absence (Hussain, 2012). Based on extensive data review conducted on different examination methods (Table 5), we also noted that wide variation exists in PL absence from 4.5-50.8% in Pan Arabs and 16.7-40.5% in Gulf Arabs (Sater et al., 2010; Hussain, 2012; Alzahrani et al., 2017; Alkhamis et al., 2017). This wide variation could be due to ethnic differences, sample size and the types of specimens or examination methods used.
A study on 136 wrists reported that the incidence of tendon absence was 10% in ultrasonography and 14% in standard physical examination methods such as Schaeffer’s test (Holzgrefe et al., 2019). In another study on 96 wrists, the tendon absence was detected for 19% by ultrasonography and 18% by physical examination methods; this study also confirmed that the Schaeffer’s is the standard test that could reliably detect PL tendon presence/absence with a sensitivity and specificity of 94% (Johnson et al., 2020). This justifies why we used only Schaeffer’s as the standard test in our study. Other than its absence, we did not observe any anomalous PL structure in our ultrasound examination, unlike the variations reported previously. Based on cadaveric dissection, it was reported that the different PL variations range from complete agenesis to changes in its location, size, shape and the insertion site (Reimann et al., 1994; Thejodhar et al., 2008). Olewnik et al. (2017) described three variant insertions of the PL and classified them as Type I, II and III. In Type I, the muscle inserted into the palmar aponeurosis (78.8% of the cases), whereas in Type II, a bifurcated muscle tendon was seen getting inserted to the palmar aponeurosis and flexor retinaculum (12.5% of cases), and in Type III, the tendon was seen fusing with the flexor carpi ulnaris and getting inserted into the palmar aponeurosis and pisiform bone (1.2% of the cases). These morphometric patterns suggest that PL is the most variable muscle in the human forearm. This high variability in its presence/absence and structure may be linked to its development, and it has been postulated that the absence of PL is hereditary and linked to the HOX gene, which is responsible for the regulation of its morphological development (Amthor et al., 1999). From our ultrasonographic examination, we also noticed statistically significant differences in terms of tendon structure among nationalities and gender. These variations could be either developmental or acquired.
A recent meta-analysis of studies suggest that the absence of PL is more common in females, especially on the left sides (Pekala et al., 2017). Our findings also suggest that the absence of PL is more frequent in females, but on the right side (Table 1). It has been argued that the functional tests are likely to overestimate the absence of PL; thus, the usage of ultrasound assessment prior to grafting is preferred (Pekala et al., 2017). This is the reason why we have used Schaeffer’s test along with ultrasound imaging. Not surprisingly, the Schaeffer’s test gave a false negative result for 11 wrists in our study (Table 1).
Studies report that the absence of PL has no adverse effects or functional disadvantages in daily activities. Due to this reason the PL tendon is often used for grafts. The tendon harvest is crucial in surgical procedures. Due to its proximity with the tendon, the median nerve is also prone for injury during this procedure, if its distance from the tendon is not assessed before the surgical procedure (Lawler and Adams, 2007). In such cases, the ultrasound findings of our study mentioning the distance between tendon and nerve are very useful for the surgeons to be aware of the risks associated during tendon harvest procedures. The distance from mid-portion of the inter-styloid area to the point where the tendon crossed the median nerve was between 2.63 mm (shortest) and 5.62 mm (greatest) (Olewnik et al., 2017). In our study, from the ultrasound images of the transverse sections, we have measured the distance of the tendon from the nerve (2cm proximal to distal wrist crease) and found that the range of distance was 1.30±0.63 mm (right side) and 1.24±0.61 mm (left side). Investigators have used different sites to measure the PL tendon using ultrasonography (Olewnik et al., 2017; Karacan et al., 2017; Johnson et al., 2018). A recent systematic review stated that the mean width (transverse diameter) of the PL tendon is 4.0±1.7 mm, ranging from 2.8 mm to 7.7 mm (Yammine and Eric, 2020). The level of the measurement reported in all those studies is different from point to point, ranging from the proximal end, midpoint and distal end of the tendon, respectively. Whereas in our study the level of measurement was 2 cm proximal to distal wrist crease and the mean width of PL tendon measured by ultrasonography was 4.08±1.34 mm and 4.36±1.26 mm on the right and left sides: 4.61±1.23 mm and 3.93±1.29 mm in male and females, respectively. The limitation of our study is that we did not do the ultrasonography of the whole muscle; we did not measure the whole length of the tendon, bearing in mind the fact that the assessment of the “PL tendon diameter” is less invasive than the “PL tendon length”, as surgically and anatomically the diameter can easily be achieved through a transverse incision at the wrist before planning tendon harvest surgery.
Conclusion
Our study has documented both the topographic and ultrasonographic features of the PL tendon in a Gulf Arab population, and confirmed that the ultrasonography is more reliable for detecting the PL tendon than the most often used clinical test: i.e., Schaeffer’s test. Our study provides the quantitative data on the diameters of the PL tendon at the wrist based on ultrasonographic assessment. These data may be helpful, especially for the surgeons in the region, for their potential application in orthopedic and reconstructive surgeries that use PL grafting.
ACKNOWLEDGEMENTS
Authors would like to thank all the students for their voluntary participation in the study. Our sincere thanks to CMMS, AGU for grant support (Grant number: G-E011-PI-11/18). We thank Dr. Ahmed Jaradat and Dr. Mohammed Ali Yunus Khan for their support in this project.
Related articles
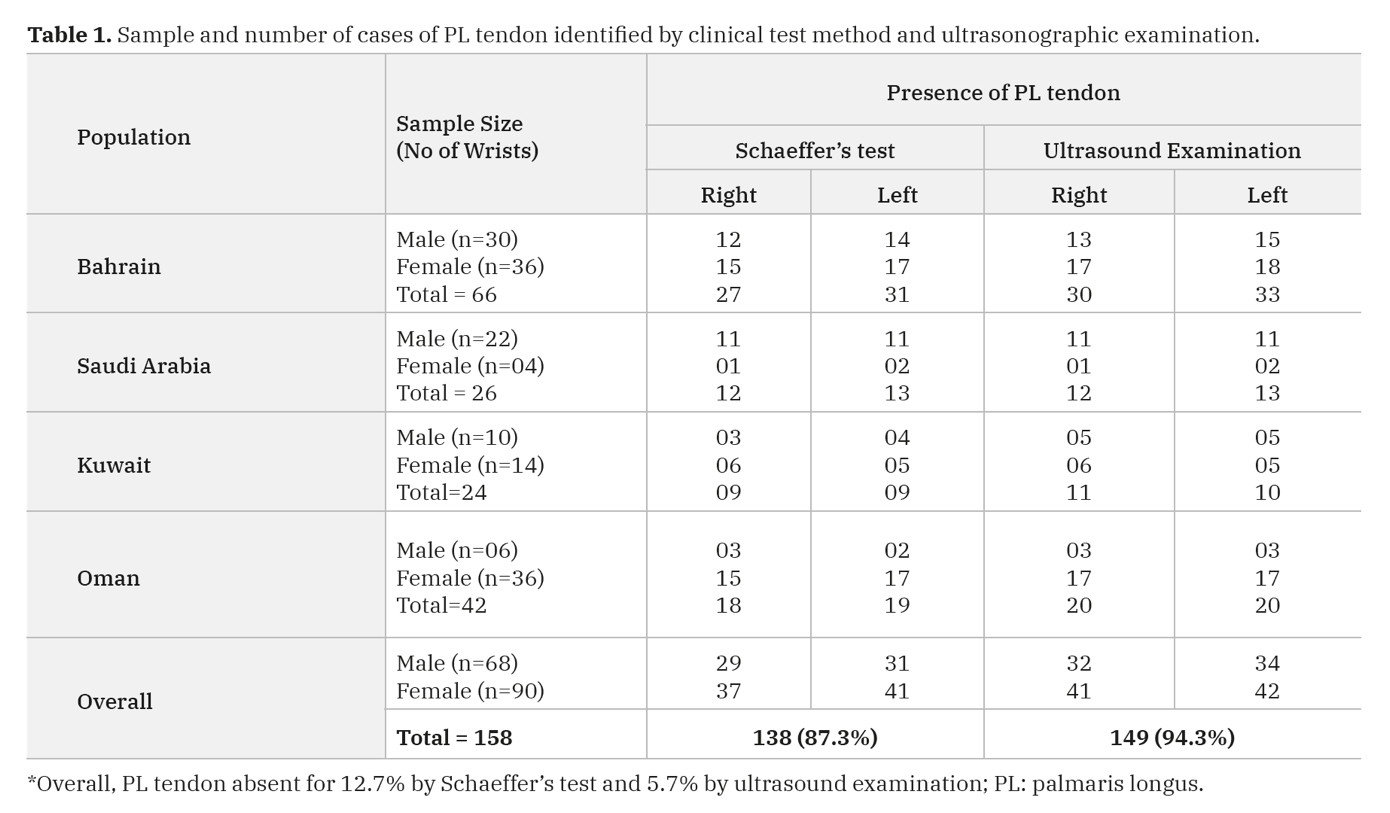 Table 1. Sample and number of cases of PL tendon identified by clinical test method and ultrasonographic examination.
Table 1. Sample and number of cases of PL tendon identified by clinical test method and ultrasonographic examination.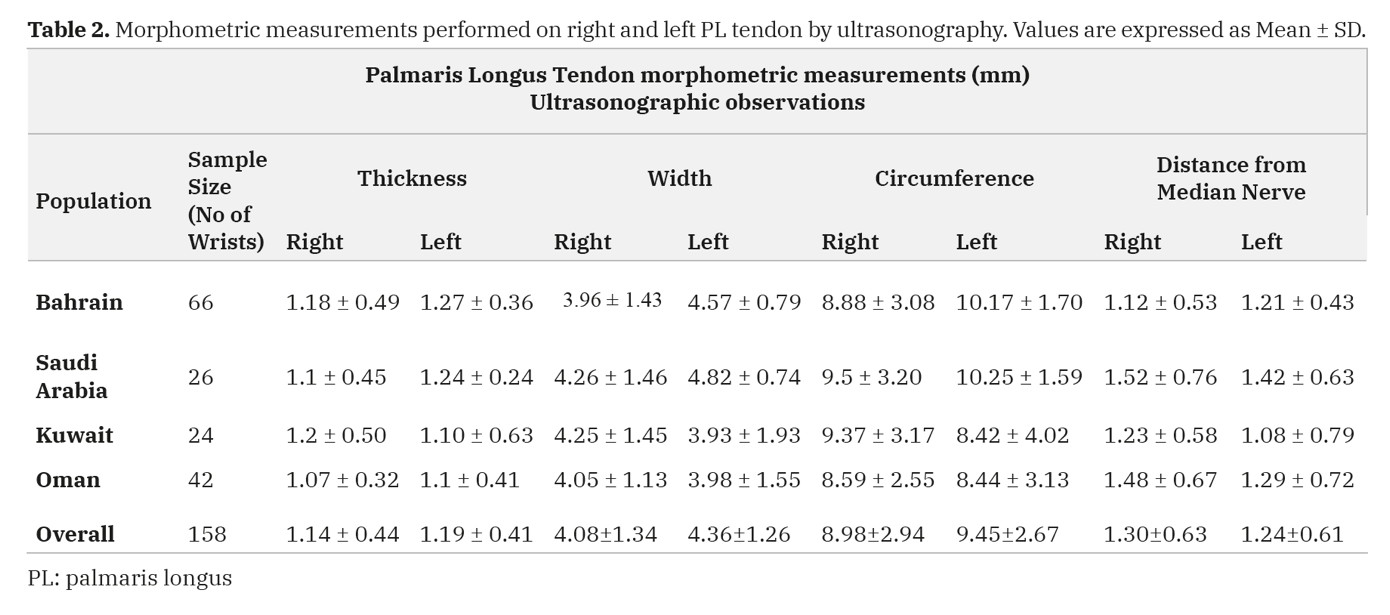 Table 2. Morphometric measurements performed on right and left PL tendon by ultrasonography. Values are expressed as Mean ± SD.
Table 2. Morphometric measurements performed on right and left PL tendon by ultrasonography. Values are expressed as Mean ± SD.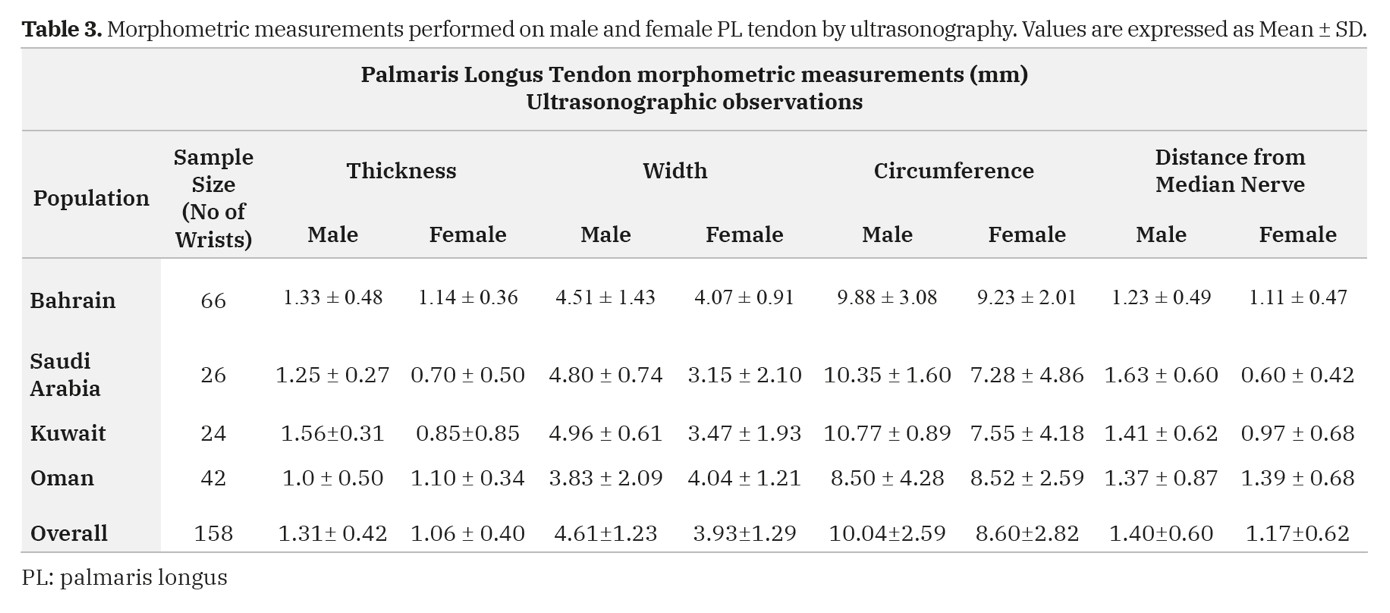 Table 3. Morphometric measurements performed on male and female PL tendon by ultrasonography. Values are expressed as Mean ± SD.
Table 3. Morphometric measurements performed on male and female PL tendon by ultrasonography. Values are expressed as Mean ± SD.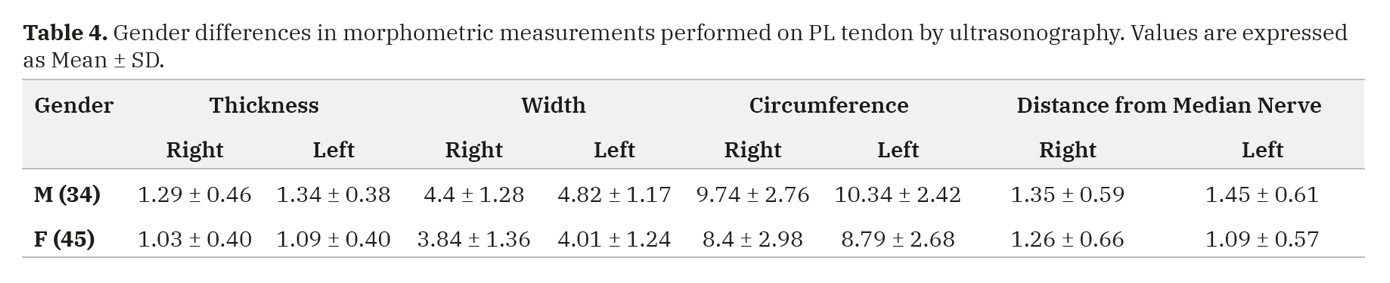 Table 4. Gender differences in morphometric measurements performed on PL tendon by ultrasonography. Values are expressed as Mean ± SD.
Table 4. Gender differences in morphometric measurements performed on PL tendon by ultrasonography. Values are expressed as Mean ± SD.ADACHI B (1909) Beiträge zur Anatomie der Japaner. XII. Die Statistik der Muskelvarietaten. Z Morph Anthropol, 12: 261-312.
AGARWAL P (2010) Absence of the palmaris longus tendon in Indian population. Indian J Orthop, 44(2): 212-215.
ALKHAMIS AA, ALSULTAN MH, ALAHMAD MS, SARAH A (2017) The frequency of palmaris longus absence among female students in King Faisal University in Al-Ahsa, Saudi Arabia. Egyptian J Hospital Med, 70 (11): 1959-1962.
ALZAHRANI MT, ALMALKI MA, ALTHUNAYAN TA, ALMOHAWIS AH, ALTURKI AT, UMEDANI L (2017) Clinical assessment of the congenital absence of palmaris longus and flexor digitorum superficialis muscles in young Saudi population. Anat Res Int, 2017: 5342497.
AMTHOR H, CHRIST B, PATEL K (1999) A molecular mechanism enabling continuous embryonic muscle growth - a balance between proliferation and differentiation. Development, 126(5): 1041-1053.
BARKATS N (2013) The prevalence of the palmaris longus muscle’s agenesis in Hungarian students. PoA, 22: 28-33.
BARKATS N (2015) Change of the agenesis rate of palmaris longus muscle in an isolated village in Ukraine. Folia Morphol, 74(4): 470-474.
BOTAR J (1931) Sur quelques variations des muscles de l’avant-bras. Bull Mem Soc Anthropol Paris, 2: 25-33.
CAETANO EB, VIEIRA LA, FERREIRA CMB, CAVALHEIRO CS, ARCURI MH, SILVA JR LCNN (2019) Anatomical study of the branch of the palmaris longus muscle for its transfer to the posterior interosseous nerve. Int J Morphol, 37(2): 626-631.
CETIN A, GENC M, SEVIL S, COBAN YK (2013) Prevalence of the palmaris longus muscle and its relationship with grip and pinch strength: a study in a Turkish pediatric population. Hand (NY), 8(2): 215-220.
CEYHAN O, MAVT A (1997) Distribution of agenesis of palmaris longus muscle in 12-18 years old age groups. Indian J Med Sci, 51(5): 156-160.
CHOO J, WILHELMI BJ, KASDAN ML (2017) Iatrogenic injury to the median nerve during palmaris longus harvest: An overview of safe harvesting techniques. Hand, 12(1): NP6-NP9.
CLEMENTE CD (1985) Anatomy of the Human Body. Lea and Febiger, Philadelphia.
DABROWSKI K, STANKIEWICZ-JOZWICKA H, KOWALCZYK A, MARKUSZEWSKI M, CISZEK B (2018) The sonographic morphology of musculus palmaris longus in humans. Folia Morphol, 77(3): 509-513.
DOWDY PA, RICHARDS RS, MCFARLANE RM (1994) The palmar cutaneous branch of the median nerve and the palmaris longus tendon: A cadaveric study. J Hand Surg Am, 19(2): 199-202.
DVORAKOWA M, ZVOLSKY P (1975) Absence of musculus palmaris longus in the Prague population. Cas Lek Cesk, 114(44): 1365-1368.
ERIC M, KOPRIVCIC I, VUCINIC N, RADIC R, KRIVOKUCA D, LEKSAN I, SELTHOFER R ( 2011) Prevalence of the palmaris longus in relation to the hand dominance. Surg Radiol Anat, 33(6): 481-484.
ERTEM K, SIGIRCI A, KARACA S, SIGIRCI A, KARAKOC Y, YOLOGLUS (2010) Ultrasonographic assessment of relationship between the palmaris longus tendon and the flexor retinacular ligament and the palmar aponeurosis of the hand. Eur J Gen Med, 7(2): 161-166.
GANGATA H (2009) The clinical surface anatomy anomalies of the palmaris longus muscle in the Black African population of Zimbabwe and a proposed new testing technique. Clin Anat, 22(2): 230-235.
GARAFFA G, SANSALONE S, RALPH DJ (2013) Penile reconstruction. Asian J Androl, 15(1): 16-19.
GEORGE R (1953) Co-incidence of palmaris longus and plantaris muscles. Anat Rec, 116(4): 521-523.
HASSAN AF, JABETI S (2008) Absence of the palmaris longus tendon in mid- eastern population. J Bahrain Med Soc, 20(2): 70-73.
HIZ O, EDIZ L, CEYLAN MF, GEZICI E, GULCU E, ERDEN M (2011) Prevalence of the absence of palmaris longus muscle assessed by a new examination test (Hiz-Ediz Test) in the population residing in the area of Van, Turkey. J Clin Exp Investig, 2(3): 254-259.
HOLZGREFE RE, ANASTASIO AT, FARLEY KX, DALY CA, MASON AR, GOTTSCHALK MB (2019) Detection of the palmaris longus tendon: physical examination versus sonography. J Hand Surg Eur Vol, 44(8): 800-804.
HUSSAIN FN (2012) Prevalence of congenital absence of palmaris longus tendon in young Jizani population of Saudi Arabia: A cross sectional study. Pak J Med Sci, 28(5): 865-869.
ITO MM, AOKI M, KIDA MY, ISHII S, KUMAKI K, TANAKA S (2001) Length and width of the tendinous portion of the palmaris longus: A cadaver study of adult Japanese. J Hand Surg Am, 26(4): 706-710.
JOHNSON CC, VUTESCU ES, MILLER TT, NWAWKA OK, LEE SK, WOLFE SW (2018) Ultrasound determination of presence, length and diameter of the palmaris longus tendon. J Hand Surg Eur Vol, 43(9): 948-953.
JOHNSON CC, ZUSSTONE E, MILLER TT, NWAWKA OK, LEE SK, WOLFE SW (2020) Clinical tests for assessing the presence and quality of the palmaris longus tendon: diagnostic accuracy of examination compared with ultrasound. J Hand Surg Eur Vol, 45(3): 292-298.
KAPOOR SK, TIWARI A, KUMAR A, BHATIA R, TANTUWAY V, KAPOOR S (2008) Clinical relevance of palmaris longus agenesis: Common anatomical aberration. Anat Sci Int, 83(1): 45-48.
KARACAN K, AKCAALAN M, BAYLAN H (2017) Evaluation of relationship between prevalence of palmaris longus muscle and handedness in Turkish population. Int J Morphol, 35(3): 1026-1030.
KIGERA JWM, MUKWAYA S (2011) Frequency of agenesis palmaris longus through clinical examination: An East African study. PLoS One, 6(12): e28997.
KOCABIYIK N, YILDIZ S, DEVELI S, OZAN H, YAZAR F (2012) Morphometric analysis of the palmaris longus muscle: A fetal study. Anatomy, 6-7: 42-47.
KOSE O, ADANIR O, CIRPAR M, KURKLU M, KOMURCU M (2009) The prevalence of absence of the palmaris longus: A study in Turkish population. Arch Orthop Trauma Surg, 129(5): 631-639.
KYUNG DS, LEE JH, CHOI IJ, KIM DK (2012) Different frequency of the absence of the palmaris longus according to assessment methods in a Korean population. Anat Cell Biol, 45(1): 53-56.
LALIT M, SINGLA RK, PIPLANI S (2014) Bifid inverted palmaris longus muscle – a case report. Eur J Anat, 18(3): 341-343.
LAWLER E, ADAMS BD (2007) Reconstruction for DRUJ instability. Hand, 2(3): 123-126.
LESLIE BM, OSTERMAN AL, WOLFE SW (2017) Inadvertent harvest of the median nerve instead of the palmaris longus tendon. J Bone Joint Surg Am, 99(14): 1173-1182.
MACHADO AB, DIDIO LJ (1967) Frequency of the musculus palmaris longus studied in vivo in some Amazon Indians. Am J Phys Anthropol, 27(1): 11-20.
MATHEW AJ, SUKUMARAN TT, JOSEPH S (2015) Versatile but temperamental: A morphological study of palmaris longus in the cadaver. J Clin Diagn Res, 9(2): AC01-AC03.
MBAKA GO, EJIWUNMI AB (2009) Prevalence of palmaris longus absence: A study in the Yoruba population. Ulster Med J, 78(2): 90-93.
MISHRA S (2001) Alternative tests in demonstrating the presence of palmaris longus. Indian J Plast Surg, 34: 12-14.
MOBARAKEH MK, PASHA MG, POOR MM (2008) Variation, length and width of tendinous portion of palmaris longus and forearm length and height: Is there a link? A cadaver study of adult Iranians. Iran J Med Sci, 33(3): 164-168.
MORAIS M, SANTOS W, MALYSZ T (2013) Agenesis of palmaris longus muscle: Is this a phenotype of variable expressivity? J Morphol Sci, 30(4): 249-253.
NAKANO T (1923) Beiträge zur Anatomie der Chinesen. Die Statistik der Muskelvarietaten. Folia Anat Jpn, 1: 273-282.
NASIRI E, POURGHASEM M, MOLADOUST H (2016) The prevalence of absence of the palmaris longus muscle tendon in the North of Iran: A comparative study. Iran Red Crescent Med J, 18(3): e22465.
O’SULLIVAN E, MITCHELL BS (2002) Association of the absence of palmaris longus tendon with an anomalous superficial palmar arch in the human hand. J Anat, 201(5): 405-408.
OLEWNIK L, WYSIADECKI G, POLGUJ M, TOPOL M (2017) Anatomic study suggests that the morphology of the plantaris tendon may be related to Achilles tendonitis. Surg Radiol Anat, 39(1): 69-75.
OSONUGA A, MAHAMA HM, BROWN AA, OSONUGA OA, SERBEH G, HARDING AN, HORMEKU AK (2012) The prevalence of palmaris longus agenesis among the Ghanaian population. Asian Pac J Trop Dis, 2: 887-889.
OZASA Y, WADA T, IBA K, YAMASHITA T (2018) Surgical treatment for partial rupture of the distal biceps tendon using palmaris longus tendon graft: A case report. Acta Orthop Traumatol, 52(4): 323-325.
PEKALA PA, HENRY BM, PEKALA JR, SKINNINGSRUD B, WALOCHA JA, BONCZAR M, TOMASZEWSKI KA (2017) Congenital absence of the palmaris longus muscle: A meta-analysis comparing cadaveric and functional studies. J Plast Reconstr Aesthet Surg: JPRAS, 70(12): 1715-1724.
PUSHPAKUMAR SB, HANSON RP, CARROLL S (2004) The ‘two finger’ sign. Clinical examination of palmaris longus (PL) tendon. Br J Plast Surg, 57(2): 184-185.
RAJANI S, PATEL S, RAJANI J, GANASVA A, DAMOR J (2013) Study of palmaris longus tendon agenesis through clinical examination in Gujarat region of India. Int J Res Med, 2(1): 83-87.
RAOUF HA, KADER GA, JARADAT A, DHARAP A, FADEL R, SALEM AH (2013) Frequency of palmaris longus absence and its association with other anatomical variations in the Egyptian population. Clin Anat, 26(5): 572-577.
REIMANN AF, DASELER EH, ANSON BJ, BEATON LE (1994) The palmaris longus muscle and tendon. A study of 1600 extremities. Anat Rec, 89(4): 495-505.
ROOHI AS, CHOON-SIAN L, SHALIMAR A, TAN GH, NAICKER AS, REHAB M (2007) A study on the absence of palmaris longus in a multiracial population. Malays Orthop J, 1(1): 26-28.
SANKAR KD, BHANU PS, JOHN SP (2011) Incidence of agenesis of palmaris longus in the Andhra population of India. Indian J Plast Surg, 44: 134-138.
SATER MS, DHARAP AS, ABU-HIJLEH MF (2010) The prevalence of absence of the palmaris longus muscle in the Bahraini population. Clin Anat, 23(8): 956-961.
SAXENA S (2013) A study on the absence/presence of the muscle Palmaris Longus in an Indian population. Int J Biomed Res, 2(1): 48-53.
SCHAEFFER JP (1909) On the variations of the palmaris longus muscle. Anat Rec, 3: 275-278.
SEBASTIN SJ, LIM AYT (2006) Clinical assessment of absence of the palmaris longus and its association with other anatomical anomalies: A Chinese population study. Ann Acad Med Singap, 35: 249-253.
SHARMA DK, SHUKLA CK, SHARMA V (2012) Clinical assessment of absence of palmaris longus muscle and its association with gender, body sides, handedness and other neighboring anomalies in a population of central India. J Anat Soc India, 61(1): 13-20.
SOLTANI AM, PERIC M, FRANCIS CS, NGUYEN TT, CHAN LS, GHIASSI A, STEVANOVIC MV, WONG AK (2012) The variation in the absence of the palmaris longus in a multiethnic population of the United States: an epidemiological study. Plast Surg Int, 2012: 282959.
THEJODHAR P, POTU BK, VASAVI RG (2008) Unusual palmaris longus muscle. Indian J Plast Surg, 41(1): 95-96.
THOMPSON JW, MCBATTS J, DANFORTH CH (1921) Hereditary and racial variations in the musculus palmaris longus. Am J Phys Anthrop, 4: 205-220.
THOMPSON NW, MOCKFORD BJ, CRAN GW (2001) Absence of the palmaris longus muscle: A population study. Ulster Med J, 70(1): 22-24.
TROHA F, BAIBAK GJ, KELLEHER JC (1990) Frequency of the palmaris longus tendon in North American Caucasians. Ann Plast Surg, 25(6): 477-478.
TRUSSLER AP, KAWAMOTO HK, WASSON KL, DICKINSON BP, JACKSON E, KEAGLE JN, JARRAHY R, BRADLEY JP (2008) Upper lip augmentation: palmaris longus tendon as an autologous filler. Plast Reconstr Surg, 121 (3): 1024-1032.
VASTAMAKI M (1987) Median nerve as free tendon graft. J Hand Surg, 12(2): 187-188.
VENTER G, VAN SCHOOR AN, BOSMAN MC (2014) Degenerative trends of the palmaris longus muscle in a South African population. Clin Anat, 27(2): 222-226.
WANG X, WEI B, LING T, HOU K (1983) Anatomy of palmaris longus and its clinical application. Hebei Med, 6: 53-55.
WEBER RV, MACKINNON SE (2007) Median nerve mistaken for palmaris longus tendon: restoration of function with sensory nerve transfers. Hand, 2(1): 1-4.
WEHBE MA (1992) Tendon graft donor sites. J Hand Surg Am, 17(6): 1130-1132.
YAMMINE K, ERIC M (2020) Morphometric analysis and surgical adequacy of palmaris longus as a tendon graft. A systematic review of cadaveric studies. Surg Radiol Anat, 42: 259-267.