INTRODUCTION
Many medical schools are substituting anatomy dissection with supplemental learning techniques that include digital learning such as virtual reality, augmented reality (AR), or mixed reality headset display (MR). Although the effectiveness of these techniques has been reported, data also suggest that digital learning may pose interference with learning (Nicholson et al., 2008; Nilsson et al., 2007; Qayumi et al., 2004; Devitt and Palmer, 1999). Most studies also focus on the knowledge of anatomy content as an outcome measure without any evidence of engagement, group learning, or social development during the anatomy lab experience (Hopkins et al., 2011). Virtual reality has recently become a popular modality for teaching anatomy because of its unique visualization capabilities; that is, virtual reality can place the user within the system or organ being studied. Another technical modality, MR, has the capability of simulating sensations while the user is immersed in a virtual environment (Izard et al., 2017). These modern methodologies have been a practical supplemental teaching resource, but their impact on assessment scores requires validation. Additionally, the participants complained of headaches, dizziness, or blurred vision while using the AR or virtual reality tools (Moro et al., 2017).
There have been reports of successful efforts to teach integrated anatomy by problem-based learning or case-based learning; however, the available data on the approach used for integrating clinical cases during anatomy teaching is scarce (Bains and Kaliski, 2019). There is no standard method of learning or teaching anatomy. This is especially true considering advancements in medical innovations and technologies. Our medical school uses a flipped-classroom method incorporated with a modified team-based approach. Traditionally, the flipped-classroom model means the students take charge of their learning by actively engaging in the class. The instructors facilitate the students’ teaching and learning by using multiple blended strategies mainly focused on student preferences and difficulty level.
At our institution, we provide students with an online recording of lectures, and valuable learning resources focused on their USMLE steps preparation. In class, the instructor chooses the strategies of student preferences to discuss the problems in teams and let them work through to find the correct answers. In addition to classes, we present the anatomy lab experience in a balanced multimodal integrated approach focusing on combining cadaveric prosections with advanced technology. Towards this attempt, we integrated the use of plastinated cadaveric materials with clinical cases, quizzes, virtual reality, Imaging, ultrasound experience (US), and prosection videos in anatomy labs in a team-based learning environment (Bains and Kaliski, 2012; Johnson et al., 2012).
This study assesses the impact of a multimodal approach using virtual technology, integrated clinical cases, plastinated prosections, and ultrasonography in integrated team-based learning in anatomy lab teaching. The hypothesis of this study is that teaching anatomy lab in a low-pressure active learning environment while using multiple integrated modalities could improve the medical students’ engagement within their teams. This team collaboration could eventually improve the effectiveness of learning anatomy and the social interactions between students.
METHODS
Our medical school runs a 4-year program where Years 1 and 2 mainly address the basic sciences integrated with clinical sciences, while in Years 3 and 4 the students rotate in clinical clerkships at the hospitals. Year 1 begins at the end of July and runs through the end of May (a total of 10 months). Year 2 begins in July and ends in March. The overall length of time for students to study the basic sciences is 18 months.
During the “Structural Integrity of Human Body” (MSK) course, the second course in Year 1, six anatomy lab sessions were created. Each session consisted of clinically integrated topics lasting four hours. Currently, the total number of medical students in a single class is 130. The students are divided randomly into groups of 10 that are called “colleges.” Each college is further divided into two teams of five students. The five students work in these teams during their basic science training, and most of the curriculum is delivered using a modified team-based learning format. Students review online recorded lectures, after which they attend in-person 30-minute flipped classroom sessions. Each flipped classroom session starts with individual and team readiness assurance tests (I-RATS and T-RATS).
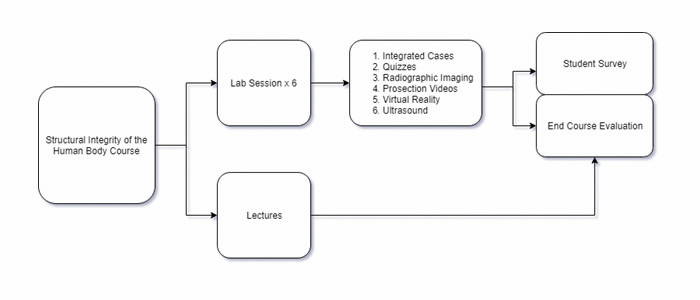
During the laboratory sessions, students worked within their groups along with their teammates. The anatomy faculty served as facilitators during the lab sessions. The histology labs were conducted in separate sections, but the content was integrated with pathology, and gross anatomy was found relevant. Each anatomy lab session contained multiple stations, lasting thirty-minutes per station (Fig. 1). Each station contained a different form of learning experience integrated with clinical thematic teaching of anatomy and the relevant clinical case of that week. These anatomy lab stations were: 1) the integrated clinical case studies on anatomy specimens, 2) embedded quizzes, 3) radiographic imaging, 4) prosection videos, 5) virtual reality, and 6) ultrasound. The quizzes consisted of checking the basic concepts of applied anatomy. The ultrasound station had handheld wireless probes connected online with the i-Pads. The Acland’s and faculty-recorded videos were made available at the video station. Students’ perceptions and comments about these experiences were collected during the end of course evaluations and an exclusive anatomy lab survey. The survey questions addressed the experience, engagement, achievement of learning outcomes, and integration between the basic science and clinical sciences.
The study protocol was approved by the Institutional Review Board of the medical school.
RESULTS
All survey studies and students’ end-of-course evaluations are collected and analyzed by the office of the assessment and evaluation and the office of continuous quality improvement. Data were collected and analyzed regarding the percent of participating students (n=88/total class n=100), who endorsed strongly disagree, disagree, neutral, agree, and strongly agree. The mode for all questions was five or "strongly agree." The questionnaire was delivered to students by email, and the office of assessment and evaluations collected all results.
The end of the course evaluations revealed that 91% of students felt the MSK course was well organized, the learning outcomes were presented (96%), and basic sciences were well integrated with clinical sciences (94%). 88% of students perceived improvement in problem-solving skills. Flipped classroom sessions enhanced their learning of clinical concepts (67%). 89% of students reported that anatomy labs enhanced their learning experience (Table 1).
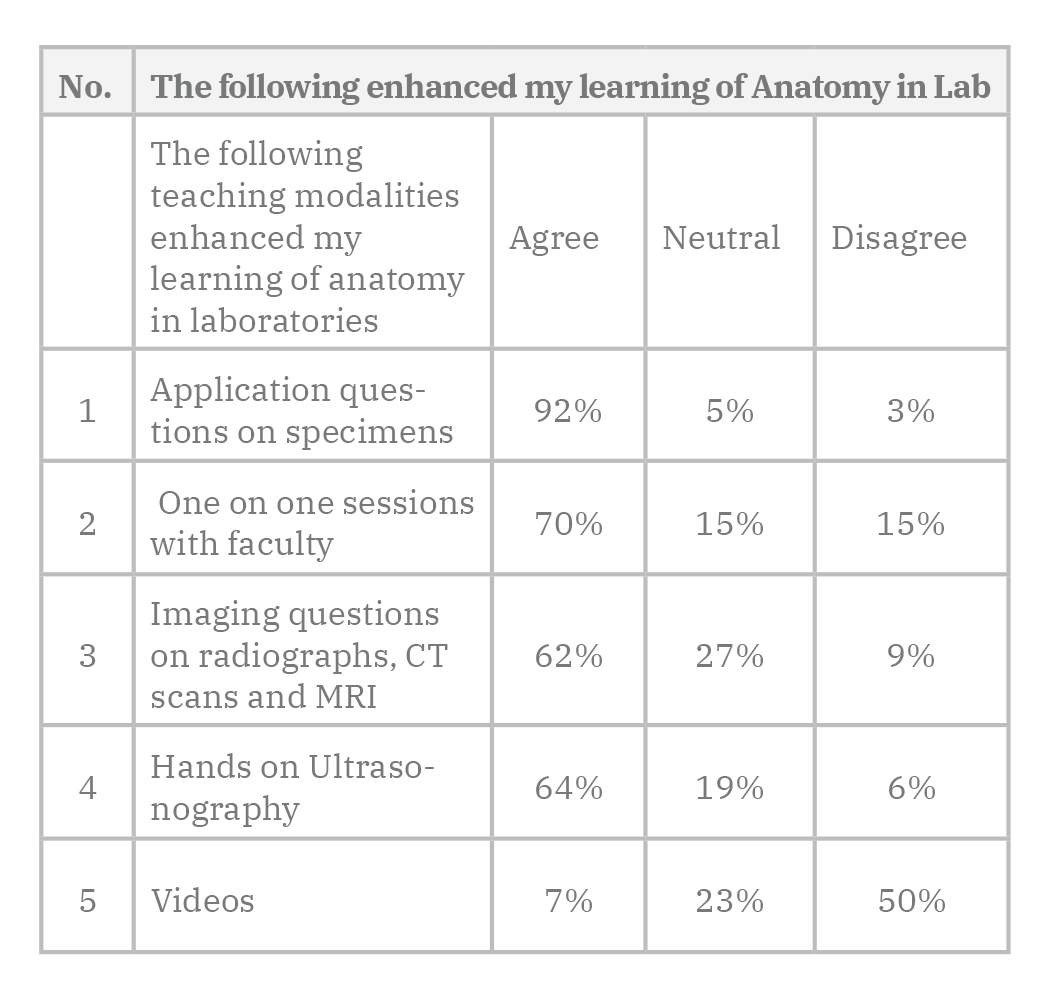
In a second survey, students were asked to compare and rate the different teaching modalities concerning the learning of anatomy in labs. 92% of students reported that application questions on anatomical specimens created the most practical anatomy learning experience. They were provided with images of CT scan, X- Rays, and MRIs combined with recall recognition and identification questions. This imaging experience was rated lower than the application question on specimens (62% vs 92%). The one-on-one faculty sessions were appreciated by many students (70%), but according to students’ perception survey about their learning, there seemed a trend that students learned more while working in groups. 64% of students agreed that the hands-on US improved their learning experience of anatomy, but the student in the US interest group was more inclined to perform the ultrasound. The dissection video watching station was rated very low in ranking; only 7% thought they were helpful to enhance the learning experience (Table 2).
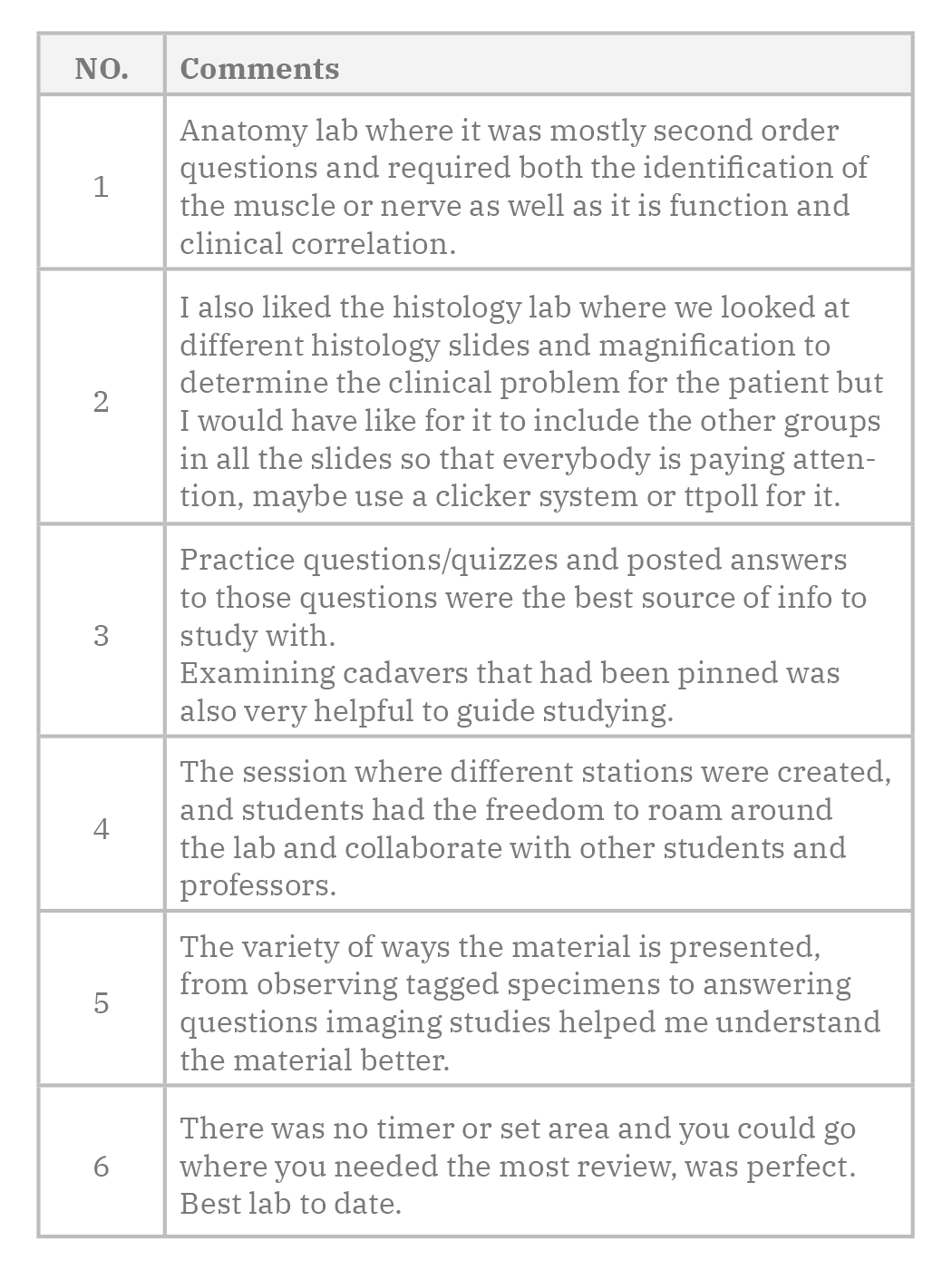
The students considered watching videos during lab hours as “a waste of time.” They suggested that videos be utilized for pre-lab preparation instead. Students commented very positively on the effectiveness of anatomy lab teaching using second-order and application questions as clinical correlates. They liked the high-yield concepts integrated within the clinical cases associated with the tagged cadaveric specimens during these lab sessions. Students liked the freedom to move around different stations and collaborate with their peers in teams (Table 3). Students also provided valuable suggestions such as inviting radiologists to these lab sessions, providing narratives to the imaging slides, adding more ultrasound lab sessions, increasing the number of integrated clinical cases at each station, facilitating interaction between teams in the lab by using technology incorporating Audience Response System clickers or online turning points.
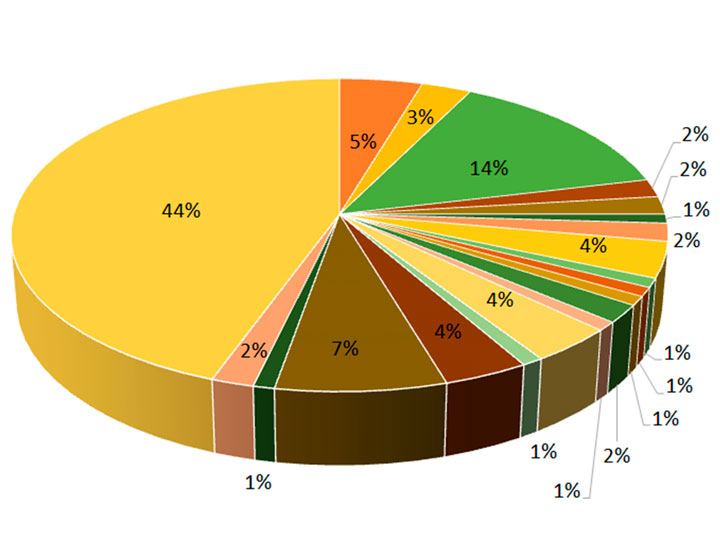
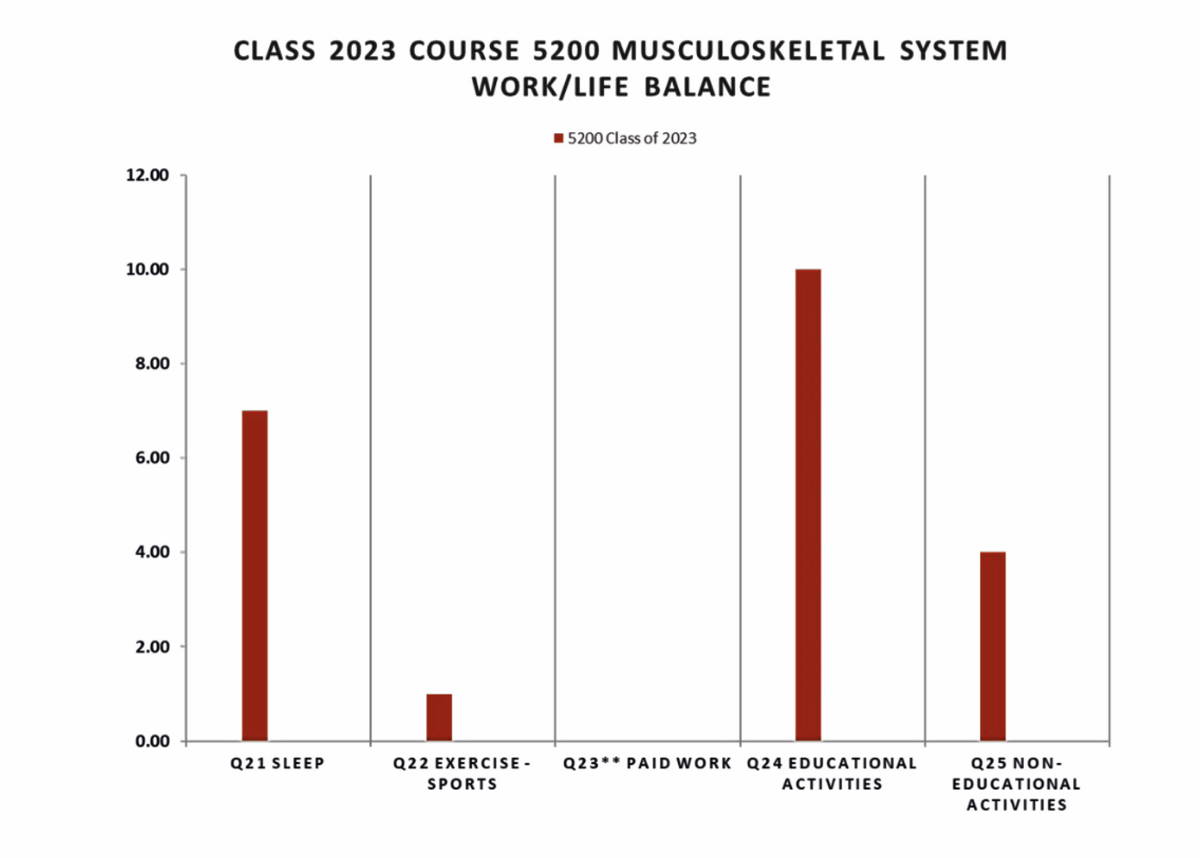
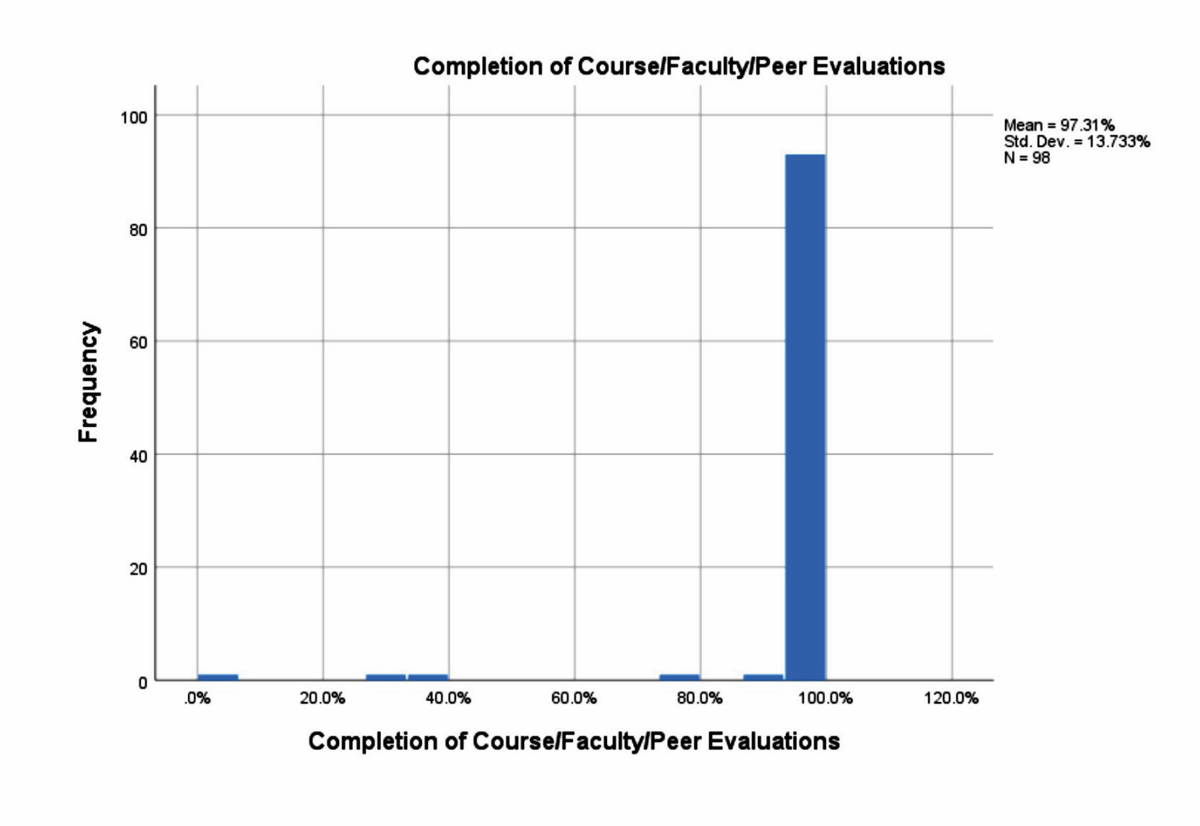
The end of course data on student’s work-life balance revealed that the average number of hours that students spent per day on sleep were seven, on exercise and support was one, on educational activities were ten, time spent with friends and family was four, and on other activities were two hours (Fig. 2). Students’ engagement was assessed by their participation in quizzes before the flipped classroom sessions via I-RATS and T-RATS. Students’ participation approached 100%, and their interest in completion of the course, faculty, and peer evaluations was 97% (Fig. 3). Bias may be considered with these figures due to the grade associated with student participation.
Faculty perceived using a multimodal approach of anatomy teaching in a team-based environment, the anatomy lab became more engaging for students. The integrated clinical cases helped students understand the clinical concept within the context of anatomy. The hands-on ultrasound experience enhanced the students’ interest and understating of anatomy. Students worked in high-performance teams with high energy and enthusiasm in a relaxed and active learning lab environment that helped improve social interaction.
DISCUSSION
Anatomy education is typically linked with cadavers, smelly dissection halls, and didactic lectures completed as a discipline by first-year medical students. While keeping some of the traditional teaching anatomy elements, most schools are approaching integrated system-based curricula (Drake, 2013). This paradigm shift takes the directions of a multimodal teaching approach, which is thought to achieve the best learning outcome as it caters to multiple learning styles (Drake and Pawlina, 2014). Instead of spending long hours in dissection and sitting in didactic lectures, the active learning pedagogies are implemented in these new curricula. Most of these teaching modalities encourage interactive learning to instruct anatomy via the team, problem, and case-based approaches (Green et al., 2014). Recent advancement in learning pedagogy is the use of a flipped-classroom approach; that is, students viewing prerecorded lectures before their in-class activities. There is strong evidence that a flipped classroom teaching approach has a significant influence on student learning compared to traditional teaching (Hew and Lo, 2018).
Our curriculum is created based on a similar philosophy of active learning using a flipped classroom, a team-based approach that was supported by the recorded lectures and classroom activities. Weekly activities include clinical presentation driven sessions with all disciplines integrated around a chosen theme per week. Flipped classroom activities are mainly focused on competency-based content delivery to promote contextual learning where students are given a reason to learn and understand concepts (Rizzolo et al., 2010). All of these factors contributed to our successful delivery of musculoskeletal system course. Students strongly agreed that learning outcomes were clearly presented, and the basic sciences were well integrated with the clinical sciences. This successful delivery was achieved because of a change in the teaching pedagogy, and faculty created flipped classroom activities to encourage student’s participation in solving the clinical problems in a team-based environment.
To enhance the learning of anatomy in a laboratory setting, the multimodal teaching approach helped the faculty succeed in achieving the learning outcome. The efficacy of an anatomy lab was improved by using the integrated clinical approach. Clinical application questions, which integrated concepts in pathology, physiology, and biochemistry, were asked while presented with anatomical specimens. Students were encouraged to work individually and then in teams to solve those clinical problems in a stepwise approach. The first part of each question was always to identify the structures and look for its location and relations. The second part of the question was to recall the neurovasculature and surrounding components in the structure of interest. The last part was to combine all the aforementioned concepts and correlate them with their clinical context. The logistics of using clinical application questions linked to the cadaveric specimens in this manner enhanced the integrated learning experience. Students were engaged and interested to pursue the next step to solve the problem. Literature suggests and supports improved student confidence when integrating anatomy knowledge clinical methods (Bradley et al., 2015).
The anatomy team also wanted to incorporate the element of integrated learning self-learning and self-assessment through formative quizzes. There is evidence that supports the positive impact of self-leaning and self-assessment that improves the knowledge, performance, and lifelong learning (Duffy and Holmboe, 2006). The answers to practice problems on specimens were discussed and uploaded to the school’s Learning Management System. There has been considerable emphasis on imaging exposure during the foundation years of medical students, but there remains controversy among anatomy faculty about the methods to teach imaging in anatomy laboratories. The question is that whether-or-not structure identification is sufficient to interpret images the way it is done in clinical practice (Marsland et al., 2018). We believed that future physicians should learn imaging in the clinical context. The labs that the anatomy team devised contained a hybrid of identification and application questions seen on most relevant medical images taken by different imaging modalities like X-Rays, Computerized Tomography (CT) scans, Magnetic resonance images (MRI), and the US. The results of the current study revealed that students appreciated incorporating radiographs in the lab with concerns about the explanation and interpretation of images. Literature supports the importance of imaging in the modern curriculum, but at the same time these sessions are required to be well planned with the collaboration of the content experts (Nwachukwu, 2014).
Functional living anatomy teaching with the US has become an important modality that has incorporated the modern curriculum to supplement the traditional cadaver-based and cross-sectional anatomy (Hoppmann et al., 2015). To enhance integrated learning, the US has been shown to promote the understanding of physiology, pathophysiology, and anatomy (Garcia de Casasola et al., 2015). Some medical schools incorporate the Point-of-Care US in their curricula to improve medical students’ diagnostic and clinical skills (Vasileios et al., 2013).
The students had hands-on ultrasonography sessions to perform the US with cordless scanners that display images on I-pads and cell phones. The required lab outcome was to identify the structures in their clinical context. Students felt very strongly about having more US sessions as they perceived it as an excellent learning resource to integrate their clinical skills and anatomy. This data is consistent with studies conducted at other established and renowned medical schools. The results of most of these studies were inclined towards creating a four-year integrated US program with more exposure in years one and two (Bahner et al., 2014). Our students believed the US sessions helped improve their perception of anatomy, which is similar to the findings in previous studies (Smith et al., 2018).
Overall the integrated labs were perceived very positively by the students. Additionally, they created a culture of improved social interaction among them. The students were actively engaged in learning by their peers who have benefited both the peer teachers and the learners (Benè and Bergus, 2014). The anatomy team plans to implement high-tech anatomy labs with state-of-the-art equipment to augment the integrated learning of anatomy.
Regarding the work-life balance, our students slept on an average of seven per 24 hours. These findings were consistent with the average requirement of sleep by a healthy adult. According to the sleep foundation, the daily sleep time averages about seven to eight hours for an adult with little variation due to the lifestyle (Sleepfoundation.org., 2020). Many studies supported increased performance, improved alertness, and mood after attaining required sleep time (Belenky et al., 2003). One study revealed a performance decrease when subjects were exposed to 13 hours of sleep or more (Taub et al., 1977). Studies have shown that sleep restriction of four hours a night can cause a significant effect on normal health, such as an increase in the heart rate or blood pressure, inflammation, obesity, or glucose tolerance. There was evidence of increase mortality in subjects who reported short sleep hours (less than seven) and long sleep hours (more than nine) (Tochikubo et al., 1996; Meier-Ewert et al., 2004; Spiegel et al., 1999; Spiegel et al., 2004; Knutson et al., 2009). Based on all these studies, we strongly encouraged our students to get enough sleep regularly and balance their studies, work, and life.
Conclusions
Integrated clinical teaching in anatomy lab provided students with a conceptual knowledge of integrated anatomy, pathology, and physiology that will prepare them for the high-stake exams and clerkship years. The integration of clinical cases with the cadaveric specimens and hands-on ultrasound elaborated the understating of contextual clinical-anatomical concepts essential for future physicians. During the anatomy lab, the relaxed, active learning environment helped students to work efficiently within their teams and improve their social interaction.
Author relevant Credit roles:
FN: Conceptualization; Data collection and analysis; original idea, study design, original draft, review and editing. FS: Conceptualization, Important intellectual contribution, data collection, critical review, data analysis. SH: Conceptualization, critical review and editing. Important intellectual contribution, data collection, and analysis.