One of the branches of the mandibular nerve is the buccal nerve. It is responsible for sensory innervating of the buccal gingiva of the lower teeth and the buccal mucosa of the cheek. The aim of this study was to report a case of a cadaver with an anatomic variation of the buccal nerve (branch of Trigeminal Nerve – V3). During a routine Anatomy class, from the observation of a 43-year-old female cadaver head, a unilateral (left side) communicating branch between the buccal branch of the trigeminal nerve and the inferior alveolar nerve was found. The knowledge of anatomical variations is essential to avoid errors and to give the patient adequate clinical management during specific dental and surgical procedures in each case.
Case report of an anatomic variation of the buccal nerve (branch of Trigeminal Nerve – V3)
Beatriz C. Ferreira1, Alexandre R. Freire1, José A.G. Junqueira2, Paulo R. Botacin2, Felippe B. Prado1, Ana C. Rossi1
1 Department of Biosciences, Anatomy Division, Piracicaba Dental School, University of Campinas, Piracicaba, São Paulo, Brazil
2 Department Basic Sciences, Araçatuba Dental School, Paulista State University, Araçatuba, São Paulo, Brazil
SUMMARY
Eur. J. Anat.
, 25
(4):
509-
513
(2021)
ISSN 2340-311X (Online)
Sign up or Login
INTRODUCTION
The trigeminal nerve is the fifth pair of cranial nerve (V) and its primary function is to give sensory and especially motor innervation to the masticatory musculature. The mandibular nerve (V3) is the third division of the trigeminal nerve (Standring, 2015). It is the only branch that carries afferent and efferent fibers. Its motor component is responsible for innervating the mandibular muscles, while the sensory component is divided to innervate the lower dental arcade, the buccal mucosa, the temporomandibular joint and the anterior two-thirds of the tongue (Standring, 2015; Huff and Daly, 2018; Ghatak and Ginglen, 2018).
One of the branches of the mandibular nerve is the buccal nerve. It is responsible for sensory innervating of the buccal gingiva of the lower dental arcade and the buccal mucosa of the cheek (Katori et al., 2012; Standring, 2015). After passing between the upper and lower heads of the lateral pterygoid muscle, it descends anteriorly in association with the maxillary artery, the temporalis muscle tendon, which is inserted into the anterior border of the mandibular ramus, and the buccal fat pad to go through the surface of the buccinator muscle (Mérida-Velasco et al., 2001; Takezawa et al., 2018). Katori et al. (2012) reported that the topographical relationship between the buccal nerve and the lateral pterygoid muscle seems to alter during fetal development, due to the delayed development of the upper head, which is much smaller than the lower head in young fetuses. The authors described that the postero-anterior nerve course seemed to be determined by a branch to the temporalis muscle (i.e., the anterior deep temporal nerve).
Descriptions regarding the distribution of the buccal nerve in Anatomy contents usually do not provide precise and detailed information about the plurality of nerve distribution variations between individuals (Takezawa et al., 2018). According to Voirol et al. (2016), the mandibular nerve, including its branches, present the most considerable anatomic variations when compared to the other cranial nerves. The buccal nerve, for example, may innervate the lower molar by reaching the alveolar bone through the retromolar foramen. It can be the reason of a failure in local anesthesia in dental procedures when doing the inferior alveolar nerve block (Ghatak and Ginglen, 2018).
The aim of this study was to report a case of a cadaver with an anatomic variation of the buccal nerve (branch of Trigeminal Nerve - V3).
CASE REPORT
During a routine Anatomy class, from the observation of a 43-years-old female cadaver head fixed in 10% formalin, in the Anatomy Laboratory of the Araçatuba Dental School, Paulista State University - UNESP of Araçatuba, SP, Brazil, a unilateral (left side) communicating branch between the buccal branch of the trigeminal nerve and the inferior alveolar nerve was found.
When the buccal nerve passes laterally to the heads of the lateral pterygoid muscle, a communicating branch was observed downward to the inferior alveolar nerve (Fig. 1). Then, this communicating branch penetrates the mandibular canal through the mandibular foramen (the mandibular ramus was removed to show the nerves) (Fig. 2). It can be observed that the inferior alveolar nerve has a loop (a branch that leaves the main trunk of the nerve and then returns to it). The origin of the loop is at the same level of the buccal nerve is passing between the superior and inferior heads of the lateral pterygoid muscle. Then, the communicating branch of the buccal nerve joins with this loop and both are incorporated into the main trunk of the inferior alveolar nerve inside the mandibular canal (Fig. 3).
DISCUSSION
Approximately 20% of the population has anatomical variations of the trigeminal nerve, and all of these are described to be related to the mandibular nerve and its branches (Ghatak and Ginglen, 2018). Comparing all the cranial nerves, the mandibular nerve, including its branches, present the most substantial anatomic variations (Voirol et al., 2016).
According to Yang et al. in 2014, when studying Korean cadavers, in all cases, the buccal nerve formed anastomosis with the lateral superior labial nerve (a branch of the infraorbital nerve) in the angular area. Consequently, the supplementary sensory component by the buccal nerve may mask a paresthesia in the angular area originated by damage to the infraorbital nerve. Thus, a differential diagnosis may be required (Yang et al., 2014).
Furthermore, the buccal nerve was related to form anastomosis with some branches of the mental nerve, supplying sensation to the skin and the mucosa over the lateral region of the lower lip (Won et al., 2014).
The retromolar foramen is a small external orifice of the retromolar canal, located in the retromolar region of the mandible and is thought to occur in a significant percentage of the population. The accessory innervation can be the reason why failures in anesthesia techniques by regional block of the inferior alveolar and buccal nerves occur (DeSantis and Liebow, 1996; Rossi et al., 2012; Voirol et al., 2016). According to Ossenberg (1987), they may be possible due to the existence of accessory innervation to the mandibular molars. Schejtman et al. (1967) performed a cadaveric study by dissections in twenty-three hemi-mandibles and by histological sections. They reported that the retromolar canal was not observed in all cases where the retromolar foramen was present, and when it occurred, its most frequent content was a myelinated nerve (observed in eight of the nine cases that were studied microscopically). There have been cases where they found blood vessels (one or more arterioles - six cases -, and one or more venules - four cases - were found) passing through the retromolar canal, accompanied or not by a myelinated nerve. Yet, there were some cases where the retromolar canal was present and they could not observe any content in it.
Shah and Mehta (2020) reviewed the literature and reported different studies of morphometric analysis of the retromolar foramen and retromolar canal in different populations. These authors verified that when the frequency of the retromolar foramen is evaluated by the cone beam computed tomography (CBCT), studies range from 5.4% to 75.4%; when the retromolar foramen is analyzed by human dry mandible, the studies showed the frequency ranging from 3.2% to 72%. And in panoramic studies the retromolar foramen frequency ranges from 3.06% to 8.8%.
Routinely, the retromolar accessory innervation occurs as a branch of the inferior alveolar nerve. One study has found that loss of sensation in the distribution of the buccal nerve happens probably because of the presence of the retromolar foramen (Singh, 1981). In this case report a retromolar foramen was not found, but the buccal nerve reached the mandibular foramen, and this anatomical variation can be responsible for a local anesthesia failure. Because of that, when assessing local anesthesia failures, dentists must have a strong working knowledge of both normal and variant human anatomy (Gamieldien and Van Schoor, 2016).
In a literature search for publications, it was found that Jablonski et al. (1985) reported an anatomic variation of the buccal nerve in which it is possible to note a unilateral origin that comes from the inferior alveolar nerve within the mandibular ramus. Besides that, no case report of an anatomical variation such as this—i.e., having a communicating branch between the buccal branch of trigeminal and the inferior alveolar nerve—was found.
In view of the anatomical variation described in the present case report, there are some factors that must be considered: which structures are innervated by the buccal nerve when passing through the mandibular canal? Is it collaborating in the innervation of structures that are normally innervated by the inferior alveolar nerve? Is the buccal nerve emitting intraosseous branches during its course through the mandibular canal? And yet, even knowing that the buccal nerve had its normal course, did the structures normally innervated by it have their innervation properly maintained?
According to Sicher and Du Brul (1970), some branches of the posterior superior alveolar nerve may innervate an area of the cheek, but they rarely substitute the normal distribution and innervation area of the buccal nerve. This corroborates, together with our findings that, despite a variant branch having emerged, the buccal nerve presented its normal path to innervate the buccal gingiva of the lower molar and the buccal mucosa of the cheek.
Thus, knowledge of anatomical variations is essential to avoid errors and to give the patient adequate clinical management during specific dental and surgical procedures in each case.
Related articles
Case report
Case report
Error: the field format must contains "%s" or "%1$s".
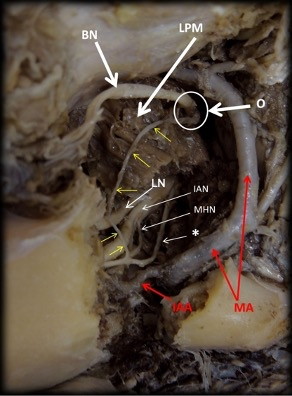 Fig. 1.- Lateral view of the mandible (left side), whose ramus was removed to expose the nerves. The communicating buccal nerve branch presented an origin (O) directly from the buccal nerve (BN), with a descendent way to join with an inferior alveolar nerve loop (*). BM: Buccinator muscle. LPM: Lateral Pterygoid Muscle. IAN: Inferior Alveolar Nerve. MHN: Milo-Hyoid Nerve. IAA: Inferior Alveolar Artery. MA: Maxillary Artery. LN: Lingual Nerve. Yellow arrows indicate the communicating buccal nerve branch.
Fig. 1.- Lateral view of the mandible (left side), whose ramus was removed to expose the nerves. The communicating buccal nerve branch presented an origin (O) directly from the buccal nerve (BN), with a descendent way to join with an inferior alveolar nerve loop (*). BM: Buccinator muscle. LPM: Lateral Pterygoid Muscle. IAN: Inferior Alveolar Nerve. MHN: Milo-Hyoid Nerve. IAA: Inferior Alveolar Artery. MA: Maxillary Artery. LN: Lingual Nerve. Yellow arrows indicate the communicating buccal nerve branch.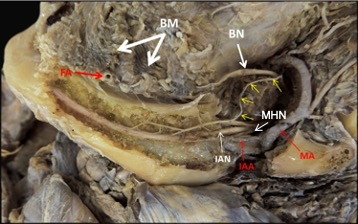 Fig. 2.- Lateral view of the mandible (left side) after removing the cortical bone to expose the internal region of the mandibular body and the branch formed by the communication of the buccal nerve (yellow arrows) and the inferior alveolar nerve loop. MA: Maxillary Artery. FA: Facial Artery. IAA: Inferior Alveolar Artery. BN: Buccal Nerve. IAN: Inferior Alveolar Nerve. MHN: Milo-Hyoid Nerve.
Fig. 2.- Lateral view of the mandible (left side) after removing the cortical bone to expose the internal region of the mandibular body and the branch formed by the communication of the buccal nerve (yellow arrows) and the inferior alveolar nerve loop. MA: Maxillary Artery. FA: Facial Artery. IAA: Inferior Alveolar Artery. BN: Buccal Nerve. IAN: Inferior Alveolar Nerve. MHN: Milo-Hyoid Nerve. Fig. 3.- Close internal view of the mandibular body (left side) after removing the cortical bone. The figure shows the branch (black arrows) formed by the communication of the buccal nerve (yellow arrow) and inferior alveolar loop (*), which join the inferior alveolar nerve (IAN) by two sites. FA: Facial Artery. IAA: Inferior Alveolar Artery. MHN: Milo-Hyoid Nerve. LN: Lingual Nerve.
Fig. 3.- Close internal view of the mandibular body (left side) after removing the cortical bone. The figure shows the branch (black arrows) formed by the communication of the buccal nerve (yellow arrow) and inferior alveolar loop (*), which join the inferior alveolar nerve (IAN) by two sites. FA: Facial Artery. IAA: Inferior Alveolar Artery. MHN: Milo-Hyoid Nerve. LN: Lingual Nerve.DESANTIS JL, LIEBOW C (1996) Four common mandibular nerve anomalies that lead to local anesthesia failures. J Am Dent Assoc, 127(7): 1081-1086.
GAMIELDIEN MY, VAN SCHOOR A (2016) Retromolar foramen: an anatomical study with clinical considerations. Br J Oral Maxillofac Surg, 54(7): 784-787.
GHATAK RN, GINGLEN JG (2018) Anatomy, Head and Neck, Mandibular Nerve. StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL).
HUFF T, DALY DT (2018) Neuroanatomy, Cranial Nerve 5 (Trigeminal). StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL).
JABLONSKI NG, CHENG CM, CHENG LC, CHEUNG HM (1985) Unusual origins of the buccal and mylohyoid nerves. Oral Surg Oral Med Oral Pathol, 60: 487-488.
KATORI Y, YAMAMOTO M, ASAKAWA S, MAKI H, RODRÍGUEZ-VÁZQUEZ JF, MURAKAMI G, ABE S (2012) Fetal developmental change in topographical relationship between the human lateral pterygoid muscle and buccal nerve. J Anat, 220(4): 384-395.
MÉRIDA-VELASCO JR, RODRÍGUEZ-VÁZQUEZ JF, DE LA CUADRA C, MÉRIDA-VELASCO JA, JIMÉNEZ-COLLADO J (2001) The course of the buccal nerve: relationships with the temporalis muscle during the prenatal period. J Anat, 198(Pt 4): 423-429.
OSSENBERG NS (1987) Retromolar foramen of the human mandible. Am J Phys Anthropol, 73(1): 119-128.
ROSSI AC, FREIRE AR, PRADO BG, PRADO FB, BOTACIN PR, CARIA PHF (2012) Incidence of retromolar foramen in human mandibles: ethnic and clinical aspects. Int J Morphol, 30(3): 1074-1078.
SCHEJTMAN R, DEVOTO FC, ARIAS NH (1967) The origin and distribution of the elements of the human mandibular retromolar canal. Arch Oral Biol, 12(11): 1261-1268.
SHAH SP, MEHTA D (2020) Mandibular retromolar foramen and canal - a systematic review and meta-analysis. Ann Maxillofacial Surg, 10(2): 444-449.
SICHER H, DU BRUL EL (1970) Oral Anatomy. 5th ed. Ishiyaku EuroAmerica: Saint Louis.
SINGH S (1981) Aberrant buccal nerve encountered at third molar surgery. Oral Surg Oral Med Oral Pathol, 52(2): 142.
STANDRING S (2015) Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 41st edition. Elsevier.
TAKEZAWA K, GHABRIEL M, TOWNSEND G (2018) The course and distribution of the buccal nerve: clinical relevance in dentistry. Aust Dent J, 63(1): 66-71.
VOIROL JR, STROTHMANN KA, ZANDIAN A, VILENSKY JA (2016) Cranial Nerves N‐VI. In: Tubbs RS, Shoja MM, Loukas M (eds). Bergman’s Comprehensive Encyclopedia of Human Anatomic Variation.
WON SY, YANG HM, WOO HS, CHANG KY, YOUN KH, KIM HJ, HU KS (2014) Neuroanastomosis and the innervation territory of the mental nerve. Clin Anat, 27(4): 598-602.
YANG HM, WON SY, LEE YI, KIM HJ, HU KS (2014) The Sihler staining study of the infraorbital nerve and its clinical complication. J Craniofac Surg, 25(6): 2209-2213.